- - Google Chrome
Intended for healthcare professionals
- My email alerts
- BMA member login
- Username * Password * Forgot your log in details? Need to activate BMA Member Log In Log in via OpenAthens Log in via your institution


Search form
- Advanced search
- Search responses
- Search blogs
- New advances in type 1...
New advances in type 1 diabetes
- Related content
- Peer review
This article has a correction. Please see:
- New advances in type 1 diabetes - June 03, 2024
- Savitha Subramanian , professor of medicine ,
- Farah Khan , clinical associate professor of medicine ,
- Irl B Hirsch , professor of medicine
- University of Washington Diabetes Institute, Division of Metabolism, Endocrinology and Nutrition, University of Washington, Seattle, WA, USA
- Correspondence to: I B Hirsch ihirsch{at}uw.edu
Type 1 diabetes is an autoimmune condition resulting in insulin deficiency and eventual loss of pancreatic β cell function requiring lifelong insulin therapy. Since the discovery of insulin more than 100 years ago, vast advances in treatments have improved care for many people with type 1 diabetes. Ongoing research on the genetics and immunology of type 1 diabetes and on interventions to modify disease course and preserve β cell function have expanded our broad understanding of this condition. Biomarkers of type 1 diabetes are detectable months to years before development of overt disease, and three stages of diabetes are now recognized. The advent of continuous glucose monitoring and the newer automated insulin delivery systems have changed the landscape of type 1 diabetes management and are associated with improved glycated hemoglobin and decreased hypoglycemia. Adjunctive therapies such as sodium glucose cotransporter-1 inhibitors and glucagon-like peptide 1 receptor agonists may find use in management in the future. Despite these rapid advances in the field, people living in under-resourced parts of the world struggle to obtain necessities such as insulin, syringes, and blood glucose monitoring essential for managing this condition. This review covers recent developments in diagnosis and treatment and future directions in the broad field of type 1 diabetes.
Introduction
Type 1 diabetes is an autoimmune condition that occurs as a result of destruction of the insulin producing β cells of the pancreatic islets, usually leading to severe endogenous insulin deficiency. 1 Without treatment, diabetic ketoacidosis will develop and eventually death will follow; thus, lifelong insulin therapy is needed for survival. Type 1 diabetes represents 5-10% of all diabetes, and diagnosis classically occurs in children but can also occur in adulthood. The burden of type 1 diabetes is expansive; it can result in long term complications, decreased life expectancy, and reduced quality of life and can add significant financial burden. Despite vast improvements in insulin, insulin delivery, and glucose monitoring technology, a large proportion of people with type 1 diabetes do not achieve glycemic goals. The massive burden of type 1 diabetes for patients and their families needs to be appreciated. The calculation and timing of prandial insulin dosing, often from food with unknown carbohydrate content, appropriate food and insulin dosing when exercising, and cost of therapy are all major challenges. The psychological realities of both acute management and the prospect of chronic complications add to the burden. Education programs and consistent surveillance for “diabetes burnout” are ideally available to everyone with type 1 diabetes.
In this review, we discuss recent developments in the rapidly changing landscape of type 1 diabetes and highlight aspects of current epidemiology and advances in diagnosis, technology, and management. We do not cover the breadth of complications of diabetes or certain unique scenarios including psychosocial aspects of type 1 diabetes management, management aspects specific to older adults, and β cell replacement therapies. Our review is intended for the clinical reader, including general internists, family practitioners, and endocrinologists, but we acknowledge the critical role that people living with type 1 diabetes and their families play in the ongoing efforts to understand this lifelong condition.
Sources and selection criteria
We did individual searches for studies on PubMed by using terms relevant to the specific topics covered in this review pertaining to type 1 diabetes. Search terms used included “type 1 diabetes” and each individual topic—diagnosis, autoantibodies, adjuvant therapies, continuous glucose monitoring, automated insulin delivery, immunotherapies, diabetic ketoacidosis, hypoglycemia, and under-resourced settings. We considered all studies published in the English language between 1 January 2001 and 31 January 2023. We selected publications outside of this timeline on the basis of relevance to each topic. We also supplemented our search strategy by a hand search of the references of key articles. We prioritized studies on each highlighted topic according to the level of evidence (randomized controlled trials (RCTs), systematic reviews and meta-analyses, consensus statements, and high quality observational studies), study size (we prioritized studies with at least 50 participants when available), and time of publication (we prioritized studies published since 2003 except for the landmark Diabetes Control and Complications Trial and a historical paper by Tuomi on diabetes autoantibodies, both from 1993). For topics on which evidence from RCTs was unavailable, we included other study types of the highest level of evidence available. To cover all important clinical aspects of the broad array of topics covered in this review, we included additional publications such as clinical reviews as appropriate on the basis of clinical relevance to both patients and clinicians in our opinion.
Epidemiology
The incidence of type 1 diabetes is rising worldwide, possibly owing to epigenetic and environmental factors. Globally in 2020 an estimated 8.7 million people were living with type 1 diabetes, of whom approximately 1.5 million were under 20 years of age. 2 This number is expected to rise to more than 17 million by 2040 ( https://www.t1dindex.org/#global ). The International Diabetes Federation estimates the global prevalence of type 1 diabetes at 0.1%, and this is likely an underestimation as diagnoses of type 1 diabetes in adults are often not accounted for. The incidence of adult onset type 1 diabetes is higher in Europe, especially in Nordic countries, and lowest in Asian countries. 3 Adult onset type 1 diabetes is also more prevalent in men than in women. An increase in prevalence in people under 20 years of age has been observed in several western cohorts including the US, 4 5 Netherlands, 6 Canada, 7 Hungary, 8 and Germany. 9
Classically, type 1 diabetes presents over the course of days or weeks in children and adolescents with polyuria, polydipsia, and weight loss due to glycosuria. The diagnosis is usually straightforward, with profound hyperglycemia (often >300 mg/dL) usually with ketonuria with or without ketoacidemia. Usually, more than one autoantibody is present at diagnosis ( table 1 ). 10 The number of islet autoantibodies combined with parameters of glucose tolerance now forms the basis of risk prediction for type 1 diabetes, with stage 3 being clinical disease ( fig 1 ). 11 The originally discovered autoantibody, islet cell antibody, is no longer used clinically owing to variability of the assay despite standardisation. 12
Autoantibody characteristics associated with increased risk of type 1 diabetes 10
- View inline

Natural history of type 1 diabetes. Adapted with permission from Insel RA, et al. Diabetes Care 2015;38:1964-74 11
- Download figure
- Open in new tab
- Download powerpoint
Half of all new cases of type 1 diabetes are now recognized as occurring in adults. 13 Misclassification due to misdiagnosis (commonly as type 2 diabetes) occurs in nearly 40% of people. 14 As opposed to typical childhood onset type 1 diabetes, progression to severe insulin deficiency, and therefore its clinical presentation in adults, is variable. The term latent autoimmune diabetes of adults (LADA) was introduced 30 years ago to identify adults who developed immune mediated diabetes. 15 An international consensus defined the diagnostic criteria for LADA as age >30 years, lack of need for insulin use for at least six months, and presence of islet cell autoantibodies. 16 However, debate as to whether the term LADA should even be used as a diagnostic term persists. The American Diabetes Association (ADA) Standards of Care note that for the purpose of classification, all forms of diabetes mediated by autoimmune β cell destruction are included in the classification of type 1 diabetes. 17 Nevertheless, they note that use of the term LADA is acceptable owing to the practical effect of heightening awareness of adults likely to have progressive autoimmune β cell destruction and thereby accelerating insulin initiation by clinicians to prevent diabetic ketoacidosis.
The investigation of adults with suspected type 1 diabetes is not always straightforward ( fig 2 ). 18 Islet cell autoantibodies such as glutamic acid decarboxylase antibody (GADA), tyrosine phosphatase IA2 antibody, and zinc transporter isoform 8 autoantibody act as markers of immune activity and can be detected in the blood with standardized assays ( table 1 ). The presence of one or more antibodies in adults with diabetes could mark the progression to severe insulin deficiency; these individuals should be considered to have type 1 diabetes. 1 Autoantibodies, especially GADA, should be measured only in people with clinically suspected type 1 diabetes, as low concentrations of GADA can be seen in type 2 diabetes and thus false positive measurements are a concern. 19 That 5-10% of cases of type 1 diabetes may occur without diabetes autoantibodies is also now clear, 20 and that the diabetes autoantibodies disappear over time is also well appreciated. 21

Flowchart for investigation of suspected type 1 diabetes in adults, based on data from white European populations. No single clinical feature in isolation confirms type 1 diabetes. The most discriminative feature is younger age at diagnosis (<35 years), with lower body mass index (<25), unintentional weight loss, ketoacidosis, and glucose >360 mg/dL at presentation. Adapted with permission from Holt RIG, et al. Diabetes Care 2021;44:2589-625 1
Genetic risk scoring (GRS) for type 1 diabetes has received attention to differentiate people whose classification is unclear. 22 23 24 Developed in 2019, the T1D-GRS2 uses 67 single nucleotide polymorphisms from known autoimmune loci and can predict type 1 diabetes in children of European and African ancestry. Although GRS is not available for routine clinical use, it may allow prediction of future cases of type 1 diabetes to allow prevention strategies with immune intervention (see below).
A major change in the type 1 diabetes phenotype has occurred over the past few decades, with an increase in obesity; the reasons for this are complex. In the general population, including people with type 1 diabetes, an epidemic of sedentary lifestyles and the “westernized diet” consisting of increased processed foods, refined sugars, and saturated fat is occurring. In people with type 1 diabetes, the overall improvement in glycemic control since the report of the Diabetes Control and Complications Trial (DCCT) in 1993 (when one or two insulin injections a day was standard therapy) has resulted in less glycosuria so that the typical patient with lower body weight is uncommon in high income countries. In the US T1D Exchange, more than two thirds of the adult population were overweight or obese. 25
Similarly, obesity in young people with type 1 diabetes has also increased over the decades. 26 The combination of autoimmune insulin deficiency with obesity and insulin resistance has received several descriptive names over the years, with this phenotype being described as double diabetes and hybrid diabetes, among others, 26 27 but no formal nomenclature in the diabetes classification exists. Many of these patients have family members with type 2 diabetes, and some patients probably do have both types of diabetes. Clinically, minimal research has been done into how this specific population responds to certain antihyperglycemic oral agents, such as glucagon-like peptide 1 (GLP-1) receptor agonists, given the glycemic, weight loss, and cardiovascular benefits seen with these agents. 28 These patients are common in most adult diabetes practices, and weight management in the presence of insulin resistance and insulin deficiency remains unclear.
Advances in monitoring
The introduction of home blood glucose monitoring (BGM) more than 45 years ago was met with much skepticism until the report of the DCCT. 29 Since then, home BGM has improved in accuracy, precision, and ease of use. 30 Today, in many parts of the world, home BGM, a static measurement of blood glucose, has been replaced by continuous glucose monitoring (CGM), a dynamic view of glycemia. CGM is superior to home BGM for glycemic control, as confirmed in a meta-analysis of 21 studies and 2149 participants with type 1 diabetes in which CGM use significantly decreased glycated hemoglobin (HbA 1c ) concentrations compared with BGM (mean difference −0.23%, 95% confidence interval −3.83 to −1.08; P<0.001), with a greater benefit if baseline HbA 1c was >8% (mean difference −0.43%, −6.04 to −3.30; P<0.001). 31 This newer technology has also evolved into a critical component of automated insulin delivery. 32
CGM is the standard for glucose monitoring for most adults with type 1 diabetes. 1 This technology uses interstitial fluid glucose concentrations to estimate blood glucose. Two types of CGM are available. The first type, called “real time CGM”, provides a continuous stream of glucose data to a receiver, mobile application, smartwatch, or pump. The second type, “intermittently scanned CGM,” needs to be scanned by a reader device or smartphone. Both of these technologies have shown improvements in HbA 1c and amount of time spent in the hypoglycemic range compared with home BGM when used in conjunction with multiple daily injections or “open loop” insulin pump therapy. 33 34 Real time CGM has also been shown to reduce hypoglycemic burden in older adults with type 1 diabetes ( table 2 ). 36 Alerts that predict or alarm with both hypoglycemia and hyperglycemia can be customized for the patient’s situation (for example, a person with unawareness of hypoglycemia would have an alert at a higher glucose concentration). Family members can also remotely monitor glycemia and be alerted when appropriate. The accuracy of these devices has improved since their introduction in 2006, so that currently available sensors can be used without a confirmation glucose concentration to make a treatment decision with insulin. However, some situations require home BGM, especially when concerns exist that the CGM does not match symptoms of hypoglycemia.
Summary of trials for each topic covered
Analysis of CGM reports retrospectively can assist therapeutic decision making both for the provider and the patient. Importantly, assessing the retrospective reports and watching the CGM in real time together offer insight to the patient with regard to insulin dosing, food choices, and exercise. Patients should be encouraged to assess their data on a regular basis to better understand their diabetes self-management. Table 3 shows standard metrics and targets for CGM data. 52 Figure 3 shows an ambulatory glucose profile.
Standardized continuous glucose monitoring metrics for adults with diabetes 52

Example of ambulatory glucose profile of 52 year old woman with type 1 diabetes and fear of hypoglycemia. CGM=continuous glucose monitoring; GMI=glucose management indicator
Improvements in technology and evidence for CGM resulting in international recommendations for its widespread use have resulted in greater uptake by people with type 1 diabetes across the globe where available and accessible. Despite this, not everyone wishes to use it; some people find wearing any device too intrusive, and for many the cost is prohibitive. These people need at the very least before meal and bedtime home BGM.
A next generation implantable CGM device (Sensionics), with an improved calibration algorithm that lasts 180 days after insertion by a healthcare professional, is available in both the EU and US. Although fingerstick glucose calibration is needed, the accuracy is comparable to that of other available devices. 53
Advances in treatments
The discovery of insulin in 1921, resulting in a Nobel Prize, was considered one of the greatest scientific achievements of the 20th century. The development of purified animal insulins in the late 1970s, followed by human insulin in the early 1980s, resulted in dramatic reductions in allergic reactions and lipoatrophy. Introduction of the first generation of insulin analogs, insulin lispro in the mid-1990s followed by insulin glargine in the early 2000s, was an important advance for the treatment of type 1 diabetes. 54 We review the next generation of insulin analogs here. Table 4 provides details on available insulins.
Pharmacokinetics of commonly used insulin preparations
Ultra-long acting basal insulins
Insulin degludec was developed with the intention of improving the duration of action and achieving a flatter profile compared with the original long acting insulin analogs, insulin glargine and insulin detemir. Its duration of action of 42 hours at steady state means that the profile is generally flat without significant day-to-day variability, resulting in less hypoglycemia compared with U-100 glargine. 39 55
When U-100 insulin glargine is concentrated threefold, its action is prolonged. 56 U-300 glargine has a different kinetic profile and is delivered in one third of the volume of U-100 glargine, with longer and flatter effects. The smaller volume of U-300 glargine results in slower and more gradual release of insulin monomers owing to reduced surface area in the subcutaneous space. 57 U-300 glargine also results in lesser hypoglycemia compared with U-100 glargine. 58
Ultra-rapid acting prandial insulins
Rapid acting insulin analogs include insulin lispro, aspart, and glulisine. With availability of insulin lispro, the hope was for a prandial insulin that better matched food absorption. However, these newer insulins are too slow to control the glucose spike seen with ingestion of a high carbohydrate load, leading to the development of insulins with even faster onset of action.
The first available ultra-rapid prandial insulin was fast acting insulin aspart. This insulin has an onset of appearance approximately twice as fast (~5 min earlier) as insulin aspart, whereas dose-concentration and dose-response relations are comparable between the two insulins ( table 4 ). 59 In adults with type 1 diabetes, mealtime and post-meal fast acting aspart led to non-inferior glycemic control compared with mealtime aspart, in combination with basal insulin. 60 Mean HbA 1c was 7.3%, 7.3%, and 7.4% in the mealtime faster aspart, mealtime aspart, and post‐meal faster aspart arms, respectively (P<0.001 for non-inferiority).
Insulin lispro-aabc is the second ultra-rapid prandial insulin. In early kinetic studies, insulin lispro-aabc appeared in the serum five minutes faster with 6.4-fold greater exposure in the first 15 minutes compared with insulin lispro. 61 The duration of exposure of the insulin concentrations in this study was 51 minutes faster with lispro-aabc. Overall insulin exposure was similar between the two groups. Clinically, lispro-aabc is non-inferior to insulin lispro, but postprandial hyperglycemia is lower with the faster acting analog. 62 Lispro-aabc given at mealtime resulted in greater improvement in post-prandial glucose (two hour post-prandial glucose −31.1 mg/dL, 95% confidence interval −41.0 to −21.2; P<0.001).
Both ultra-rapid acting insulins can be used in insulin pumps. Lispro-aabc tends to have more insertion site reactions than insulin lispro. 63 A meta-analysis including nine studies and 1156 participants reported increased infusion set changes on rapid acting insulin analogs (odds ratio 1.60, 95% confidence interval 1.26 to 2.03). 64
Pulmonary inhaled insulin
The quickest acting insulin is pulmonary inhaled insulin, with an onset of action of 12 minutes and a duration of 1.5-3 hours. 65 When used with postprandial supplemental dosing, glucose control is improved without an increase in hypoglycemia. 66
Insulin delivery systems
Approved automated insulin delivery systems.
CGM systems and insulin pumps have shown improvement in glycemic control and decreased risk of severe hypoglycemia compared with use of self-monitoring of blood glucose and multiple daily insulin injections in type 1 diabetes. 67 68 69 Using CGM and insulin pump together (referred to as sensor augmented pump therapy) only modestly improves HbA 1c in patients who have high sensor wear time, 70 71 but the management burden of diabetes does not decrease as frequent user input is necessary. Thus emerged the concept of glucose responsive automated insulin delivery (AID), in which data from CGM can inform and allow adjustment of insulin delivery.
In the past decade, exponential improvements in CGM technologies and refined insulin dosing pump algorithms have led to the development of AID systems that allow for minimization of insulin delivery burden. The early AID systems reduced hypoglycemia risk by automatically suspending insulin delivery when glucose concentrations dropped to below a pre-specified threshold but did not account for high glucose concentrations. More complex algorithms adjusting insulin delivery up and down automatically in response to real time sensor glucose concentrations now allow close replication of normal endocrine pancreatic physiology.
AID systems (also called closed loop or artificial pancreas systems) include three components—an insulin pump that continuously delivers rapid acting insulin, a continuous glucose sensor that measures interstitial fluid glucose at frequent intervals, and a control algorithm that continuously adjusts insulin delivery that resides in the insulin pump or a smartphone application or handheld device ( fig 4 ). All AID systems that are available today are referred to as “hybrid” closed loop (HCL) systems, as users are required to manually enter prandial insulin boluses and signal exercise, but insulin delivery is automated at night time and between meals. AID systems, regardless of the type used, have shown benefit in glycemic control and cost effectiveness, improve quality of life by improving sleep quality, and decrease anxiety and diabetes burden in adults and children. 72 73 74 Limitations to today’s HCL systems are primarily related to pharmacokinetics and pharmacodynamics of available analog insulins and accuracy of CGM in extremes of blood glucose values. The iLet bionic pancreas, cleared by the US Food and Drug Administration (FDA) in May 2023, is an AID system that determines all therapeutic insulin doses for an individual on the basis of body weight, eliminating the need for calculation of basal rates, insulin to carbohydrate ratios, blood glucose corrections, and bolus dose. The control algorithms adapt continuously and autonomously to the individual’s insulin needs. 38 Table 5 lists available AID systems.

Schematic of closed loop insulin pump technology. The continuous glucose monitor senses interstitial glucose concentrations and sends the information via Bluetooth to a control algorithm hosted on an insulin pump (or smartphone). The algorithm calculates the amount of insulin required, and the insulin pump delivers rapid acting insulin subcutaneously
Comparison of commercially available hybrid closed loop systems 75
Unapproved systems
Do-it-yourself (DIY) closed loop systems—DIY open artificial pancreas systems—have been developed by people with type 1 diabetes with the goal of self-adjusting insulin by modifying their individually owned devices. 76 These systems are built by the individual using an open source code widely available to anyone with compatible medical devices who is willing and able to build their own system. DIY systems are used by several thousand people across the globe but are not approved by regulatory bodies; they are patient-driven and considered “off-label” use of technology with the patient assuming full responsibility for their use. Clinicians caring for these patients should ensure basic diabetes skills, including pump site maintenance, a knowledge of how the chosen system works, and knowing when to switch to “manual mode” for patients using an artificial pancreas system of any kind. 76 The small body of studies on DIY looping suggests improvement in HbA 1c , increased time in range, decreased hypoglycemia and glucose variability, improvement in night time blood glucose concentrations, and reduced mental burden of diabetes management. 77 78 79 Although actively prescribing or initiating these options is not recommended, these patients should be supported by clinical teams; insulin prescription should not be withheld, and, if initiated by the patient, unregulated DIY options should be openly discussed to ensure open and transparent relationships. 78
In January 2023, the US FDA cleared the Tidepool Loop app, a DIY AID system. This software will connect the CGM, insulin pump, and Loop algorithm, but no RCTs using this method are available.
β cell replacement therapies
For patients with type 1 diabetes who meet specific clinical criteria, β cell replacement therapy using whole pancreas or pancreatic islet transplantation can be considered. Benefits of transplantation include immediate cessation of insulin therapy, attainment of euglycemia, and avoidance of hypoglycemia. Additional benefits include improved quality of life and stabilization of complications. 80 Chronic immunosuppression is needed to prevent graft rejection after transplantation.
Pancreas transplantation
Whole pancreas transplantation, first performed in 1966, involves complex abdominal surgery and lifelong immunosuppressive therapy and is limited by organ donor availability. Today, pancreas transplants are usually performed simultaneously using two organs from the same donor (simultaneous pancreas-kidney transplant (SPKT)), sequentially if the candidate has a living donor for renal transplantation (pancreas after kidney transplant (PAKT)) or on its own (pancreas transplantation alone). Most whole pancreas transplants are performed with kidney transplantation for end stage diabetic kidney disease. Pancreas graft survival at five years after SPKT is 80% and is superior to that with pancreas transplants alone (62%) or PAKT (67%). 81 Studies from large centers where SPKT is performed show that recipients can expect metabolic improvements including amelioration of problematic hypoglycemia for at least five years. 81 The number of pancreas transplantations has steadily decreased in the past two decades.
Islet transplantation
Islet transplantation can be pursued in selected patients with type 1 diabetes marked by unawareness of hypoglycemia and severe hypoglycemic episodes, to help restore the α cell response critical for responding to hypoglycemia. 82 83 Islet transplantation involves donor pancreas procurement with subsequent steps to isolate, purify, culture, and infuse the islets. Multiple donors are needed to provide enough islet cells to overcome islet cell loss during transplantation. Survival of the islet grafts, limited donor supply, and lifelong need for immunosuppressant therapy remain some of the biggest challenges. 84 Islet transplantation remains experimental in the US and is offered in a few specialized centers in North America, some parts of Europe, and Australia. 85
Disease modifying treatments for β cell preservation
Therapies targeting T cells, B cells, and cytokines that find use in a variety of autoimmune diseases have also been applied to type 1 diabetes. The overarching goal of immune therapies in type 1 diabetes is to prevent or delay the loss of functional β cell mass. Studies thus far in early type 1 diabetes have not yet successfully shown reversal of loss of C peptide or maintenance of concentrations after diagnosis, although some have shown preservation or slowing of loss of β cells. This suggests that a critical time window of opportunity exists for starting treatment depending on the stage of type 1 diabetes ( fig 1 ).
Teplizumab is a humanized monoclonal antibody against the CD3 molecule on T cells; it is thought to modify CD8 positive T lymphocytes, key effector cells that mediate β cell death and preserves regulatory T cells. 86 Teplizumab, when administered to patients with new onset of type 1 diabetes, was unable to restore glycemia despite C peptide preservation. 87 However, in its phase II prevention study of early intervention in susceptible individuals (at least two positive autoantibodies and an abnormal oral glucose tolerance test at trial entry), a single course of teplizumab delayed progression to clinical type 1 diabetes by about two years ( table 2 ). 43 On the basis of these results, teplizumab received approval in the US for people at high risk of type 1 diabetes in November 2022. 88 A phase III trial (PROTECT; NCT03875729 ) to evaluate the efficacy and safety of teplizumab versus placebo in children and adolescents with new diagnosis of type 1 diabetes (within six weeks) is ongoing. 89
Thus far, targeting various components of the immune response has been attempted in early type 1 diabetes without any long term beneficial effects on C peptide preservation. Co-stimulation blockade using CTLA4-Ig abatacept, a fusion protein that interferes with co-stimulation needed in the early phases of T cell activation that occurs in type 1 diabetes, is being tested for efficacy in prevention of type 1 diabetes ( NCT01773707 ). 90 Similarly, several cytokine directed anti-inflammatory targets (interleukin 6 receptor, interleukin 1β, tumor necrosis factor ɑ) have not shown any benefit.
Non-immunomodulatory adjunctive therapies
Adjunctive therapies for type 1 diabetes have been long entertained owing to problems surrounding insulin delivery, adequacy of glycemic management, and side effects associated with insulin, especially weight gain and hypoglycemia. At least 50% of adults with type 1 diabetes are overweight or obese, presenting an unmet need for weight management in these people. Increased cardiovascular risk in these people despite good glycemic management presents additional challenges. Thus, use of adjuvant therapies may tackle these problems.
Metformin, by decreasing hepatic glucose production, could potentially decrease fasting glucose concentrations. 91 It has shown benefit in reducing insulin doses and possibly improving metabolic control in obese/overweight people with type 1 diabetes. A meta-analysis of 19 RCTs suggests short term improvement in HbA 1c that is not sustained after three months and is associated with higher incidence of gastrointestinal side effects. 92 No evidence shows that metformin decreases cardiovascular morbidity in type 1 diabetes. Therefore, owing to lack of conclusive benefit, addition of metformin to treatment regimens is not recommended in consensus guidelines.
Glucagon-like peptide receptor agonists
Endogenous GLP-1 is an incretin hormone secreted from intestinal L cells in response to nutrient ingestion and enhances glucose induced insulin secretion, suppresses glucagon secretion, delays gastric emptying, and induces satiety. 93 GLP-1 promotes β cell proliferation and inhibits apoptosis, leading to expansion of β cell mass. GLP-1 secretion in patients with type 1 diabetes is similar to that seen in people without diabetes. Early RCTs of liraglutide in type 1 diabetes resulted in weight loss and modest lowering of HbA 1c ( table 2 ). 49 50 Liraglutide 1.8 mg in people with type 1 diabetes and higher body mass index decreased HbA 1c , weight, and insulin requirements with no increased hypoglycemia risk. 94 However, on the basis of results from a study of weekly exenatide that showed similar results, these effects may not be sustained. 51 A meta-analysis of 24 studies including 3377 participants showed that the average HbA 1c decrease from GLP-1 receptor agonists compared with placebo was highest for liraglutide 1.8 mg daily (−0.28%, 95% confidence interval −0.38% to−0.19%) and exenatide (−0.17%, −0.28% to 0.02%). The estimated weight loss from GLP-1 receptor agonists compared with placebo was −4.89 (−5.33 to−4.45) kg for liraglutide 1.8 mg and −4.06 (−5.33 to−2.79) kg for exenatide. 95 No increase in severe hypoglycemia was seen (odds ratio 0.67, 0.43 to 1.04) but therapy was associated with higher levels of nausea. GLP-1 receptor agonist use may be beneficial for weight loss and reducing insulin doses in a subset of patients with type 1 diabetes. GLP-1 receptor agonists are not a recommended treatment option in type 1 diabetes. Semaglutide is being studied in type 1 diabetes in two clinical trials ( NCT05819138 ; NCT05822609 ).
Sodium-glucose cotransporter inhibitors
Sodium-glucose cotransporter 2 (SGLT-2), a protein expressed in the proximal convoluted tubule of the kidney, reabsorbs filtered glucose; its inhibition prevents glucose reabsorption in the tubule and increases glucose excretion by the kidney. Notably, the action of these agents is independent of insulin, so this class of drugs has potential as adjunctive therapy for type 1 diabetes. Clinical trials have shown significant benefit in cardiovascular and renal outcomes in type 2 diabetes; therefore, significant interest exists for use in type 1 diabetes. Several available SGLT-2 inhibitors have been studied in type 1 diabetes and have shown promising results with evidence of decreased total daily insulin dosage, improvement in HbA 1c , lower rates of hypoglycemia, and decrease in body weight; however, these effects do not seem to be sustained at one year in clinical trials and seem to wane with time. Despite beneficial effects, increased incidence of diabetic ketoacidosis has been observed in all trials, is a major concern, and is persistent despite educational efforts. 96 97 98 Low dose empagliflozin (2.5 mg) has shown lower rates of diabetic ketoacidosis in clinical trials ( table 2 ). 47 Favorable risk profiles have been noted in Japan, the only market where SGLT-2 inhibitors are approved for adjunctive use in type 1 diabetes. 99 In the US, SGLT-2 inhibitors are approved for use in type 2 diabetes only. In Europe, although dapagliflozin was approved for use as adjunct therapy to insulin in adults with type 1 diabetes, the manufacturer voluntarily withdrew the indication for the drug in 2021. 100 Sotagliflozin is a dual SGLT-1 and SGLT-2 inhibitor that decreases renal glucose reabsorption through systemic inhibition of SGLT-2 and decreases glucose absorption in the proximal intestine by SGLT-1 inhibition, blunting and delaying postprandial hyperglycemia. 101 Studies of sotagliflozin in type 1 diabetes have shown sustained HbA 1c reduction, weight loss, lower insulin requirements, lesser hypoglycemia, and more diabetic ketoacidosis relative to placebo. 102 103 104 The drug received authorization in the EU for use in type 1 diabetes, but it is not marketed there. Although SGLT inhibitors are efficacious in type 1 diabetes management, the risk of diabetic ketoacidosis is a major limitation to widespread use of these agents.
Updates in acute complications of type 1 diabetes
Diabetic ketoacidosis.
Diabetic ketoacidosis is a serious and potentially fatal hyperglycemic emergency accompanied by significant rates of mortality and morbidity as well as high financial burden for healthcare systems and societies. In the past decade, increasing rates of diabetic ketoacidosis in adults have been observed in the US and Europe. 105 106 This may be related to changes in the definition of diabetic ketoacidosis, use of medications associated with higher risk, and admission of patients at lower risk. 107 In a US report of hospital admissions with diabetic ketoacidosis, 53% of those admitted were between the ages of 18 and 44, with higher rates in men than in women. 108 Overall, although mortality from diabetic ketoacidosis in developed countries remains low, rates have risen in people aged >60 and in those with coexisting life threatening illnesses. 109 110 Recurrent diabetic ketoacidosis is associated with a substantial mortality rate. 111 Frequency of diabetic ketoacidosis increases with higher HbA 1c concentrations and with lower socioeconomic status. 112 Common precipitating factors include newly diagnosed type 1 diabetes, infection, poor adherence to insulin, and an acute cardiovascular event. 109
Euglycemic diabetic ketoacidosis refers to the clinical picture of an increased anion gap metabolic acidosis, ketonemia, or significant ketonuria in a person with diabetes without significant glucose elevation. This can be seen with concomitant use of SGLT-2 inhibitors (currently not indicated in type 1 diabetes), heavy alcohol use, cocaine use, pancreatitis, sepsis, and chronic liver disease and in pregnancy 113 Treatment is similar to that for hyperglycemic diabetic ketoacidosis but can require earlier use and greater concentrations of a dextrose containing fluid for the insulin infusion in addition to 0.9% normal saline resuscitation fluid. 114
The diagnosis of diabetic ketoacidosis has evolved from a gluco-centric diagnosis to one requiring hyperketonemia. By definition, independent of blood glucose, a β-hydroxybutyrate concentration >3 mmol/L is required for diagnosis. 115 However, the use of this ketone for assessment of the severity of the diabetic ketoacidosis is controversial. 116 Bedside β-hydroxybutyrate testing during treatment is standard of care in many parts of the world (such as the UK) but not others (such as the US). Concerns have been raised about accuracy of bedside β-hydroxybutyrate meters, but this is related to concentrations above the threshold for diabetic ketoacidosis. 116
Goals for management of diabetic ketoacidosis include restoration of circulatory volume, correction of electrolyte imbalances, and treatment of hyperglycemia. Intravenous regular insulin infusion is the standard of care for treatment worldwide owing to rapidity of onset of action and rapid resolution of ketonemia and hyperglycemia. As hypoglycemia and hypokalemia are more common during treatment, insulin doses are now recommended to be reduced from 0.1 u/kg/h to 0.05 u/kg/h when glucose concentrations drop below 250 mg/dL or 14 mM. 115 Subcutaneous rapid acting insulin protocols have emerged as alternative treatments for mild to moderate diabetic ketoacidosis. 117 Such regimens seem to be safe and have the advantages of not requiring admission to intensive care, having lower rates of complications related to intravenous therapy, and requiring fewer resources. 117 118 Ketonemia and acidosis resolve within 24 hours in most people. 115 To prevent rebound hyperglycemia, the transition off an intravenous insulin drip must overlap subcutaneous insulin by at least two to four hours. 115
Hypoglycemia
Hypoglycemia, a common occurrence in people with type 1 diabetes, is a well appreciated effect of insulin treatment and occurs when blood glucose falls below the normal range. Increased susceptibility to hypoglycemia from exogenous insulin use in people with type 1 diabetes results from multiple factors, including imperfect subcutaneous insulin delivery tools, loss of glucagon within a few years of diagnosis, progressive impairment of the sympatho-adrenal response with repeated hypoglycemic episodes, and eventual development of impaired awareness. In 2017 the International Hypoglycemia Study Group developed guidance for definitions of hypoglycemia; on the basis of this, a glucose concentration of 3.0-3.9 mmol/L (54-70 mg/dL) was designated as level 1 hypoglycemia, signifying impending development of level 2 hypoglycemia—a glucose concentration <3 mmol/L (54 mg/dL). 119 120 At approximately 54 mg/dL, neuroglycopenic hypoglycemia symptoms, including vision and behavior changes, seizures, and loss of consciousness, begin to occur as a result of glucose deprivation of neurons in the central nervous system. This can eventually lead to cerebral dysfunction at concentrations <50 mg/dL. 121 Severe hypoglycemia (level 3), denoting severe cognitive and/or physical impairment and needing external assistance for recovery, is a common reason for emergency department visits and is more likely to occur in people with lower socioeconomic status and with the longest duration of diabetes. 112 Prevalence of self-reported severe hypoglycemia is very high according to a global population study that included more than 8000 people with type 1 diabetes. 122 Severe hypoglycemia occurred commonly in younger people with suboptimal glycemia according to a large electronic health record database study in the US. 123 Self- reported severe hypoglycemia is associated with a 3.4-fold increase in mortality. 124 125
Acute consequences of hypoglycemia include impaired cognitive function, temporary focal deficits including stroke-like symptoms, and memory deficits. 126 Cardiovascular effects including tachycardia, arrhythmias, QT prolongation, and bradycardia can occur. 127 Hypoglycemia can impair many activities of daily living, including motor vehicle safety. 128 In a survey of adults with type 1 diabetes who drive a vehicle at least once a week, 72% of respondents reported having hypoglycemia while driving, with around 5% reporting a motor vehicle accident due to hypoglycemia in the previous two years. 129 This contributes to the stress and fear that many patients face while grappling with the difficulties of ongoing hypoglycemia. 130
Glucagon is highly efficacious for the primary treatment of severe hypoglycemia when a patient is unable to ingest carbohydrate safely, but it is unfortunately under-prescribed and underused. 131 132 Availability of nasal, ready to inject, and shelf-stable liquid glucagon formulations have superseded the need for reconstituting older injectable glucagon preparations before administration and are now preferred. 133 134 Real time CGM studies have shown a decreased hypoglycemic exposure in people with impaired awareness without a change in HbA 1c . 34 135 136 137 138 CGM has shown benefit in decreasing hypoglycemia across the lifespan, including in teens, young adults, and older people. 36 139 Although CGM reduces the burden of hypoglycemia including severe hypoglycemia, it does not eliminate it; overall, such severe level 3 hypoglycemia rates in clinical trials are very low and hard to decipher in the real world. HCL insulin delivery systems integrated with CGM have been shown to decrease hypoglycemia. Among available rapid acting insulins, ultra-rapid acting lispro (lispro-aabc) seems to be associated with less frequent hypoglycemia in type 1 diabetes. 140 141
As prevention of hypoglycemia is a crucial aspect of diabetes management, formal training programs to increase awareness and education on avoidance of hypoglycemia, such as the UK’s Dose Adjustment for Normal Eating (DAFNE), have been developed. 142 143 This program has shown fewer severe hypoglycemia (mean 1.7 (standard deviation 8.5) episodes per person per year before training to 0.6 (3.7) episodes one year after training) and restoration of recognition of hypoglycemia in 43% of people reporting unawareness. Clinically relevant anxiety and depression fell from 24.4% to 18.0% and from 20.9% to 15.5%, respectively. A structured education program with cognitive and psychotherapeutic aspects for changing hypoglycemia related behaviors, called the Hypoglycemia Awareness Restoration Program despite optimized self-care (HARPdoc), showed a positive effect on changing unhelpful beliefs around hypoglycemia and improved diabetes related and general distress and anxiety scores. 144
Management in under-resourced settings
According to a recent estimate from the International Diabetes Federation, 1.8 million people with type 1 diabetes live in low and middle income countries (LMICs). 2 In many LMICs, the actual burden of type 1 diabetes remains unknown and material resources needed to manage type 1 diabetes are lacking. 145 146 Health systems in these settings are underequipped to tackle the complex chronic disease that is type 1 diabetes. Few diabetes and endocrinology specialist physicians are available owing to lack of specific postgraduate training programs in many LMICs; general practitioners with little to no clinical experience in managing type 1 diabetes care for these patients. 146 This, along with poor availability and affordability of insulin and lack of access to technology, results in high mortality rates. 147 148 149 In developed nations, low socioeconomic status is associated with higher levels of mortality and morbidity for adults with type 1 diabetes despite access to a universal healthcare system. 150 Although global governments have committed to universal health coverage and therefore widespread availability of insulin, it remains very far from realization in most LMICs. 151
Access to technology is patchy and varies globally. In the UST1DX, CGM use was least in the lowest fifth of socioeconomic status. 152 Even where technology is available, successful engagement does not always occur. 153 In a US cohort, lower CGM use was seen in non-Hispanic Black children owing to lower rates of device initiation and higher rates of discontinuation. 154 In many LMICs, blood glucose testing strips are not readily available and cost more than insulin. 151 In resource limited settings, where even diagnosis, basic treatments including insulin, syringes, and diabetes education are limited, use of CGM adds additional burden to patients. Need for support services and the time/resources needed to download and interpret data are limiting factors from a clinician’s perspective. Current rates of CGM use in many LMICs are unknown.
Inequities in the availability of and access to certain insulin formulations continue to plague diabetes care. 155 In developed countries such as the US, rising costs have led to insulin rationing by around 25% of people with type 1 diabetes. 156 LMICs have similar trends while also remaining burdened by disproportionate mortality and complications from type 1 diabetes. 155 157 With the inclusion of long acting insulin analogs in the World Health Organization’s Model List of Essential Medicines in 2021, hope has arisen that these will be included as standard of care across the world. 158 In the past, the pricing of long acting analogs has limited their use in resource poor settings 159 ; however, their inclusion in WHO’s list was a major step in improving their affordability. 158 With the introduction of lower cost long acting insulin biosimilars, improved access to these worldwide in the future can be anticipated. 160
Making insulin available is not enough on its own to improve the prognosis for patients with diabetes in resource poor settings. 161 Improved healthcare infrastructure, better availability of diabetes supplies, and trained personnel are all critical to improving type 1 diabetes care in LMICs. 161 Despite awareness of limitations and barriers, a clear understanding of how to implement management strategies in these settings is still lacking. The Global Diabetes Compact was launched in 2021 with the goal of increasing access to treatment and improving outcomes for people with diabetes across the globe. 162
Emerging technologies and treatments
Monitoring systems.
The ability to measure urinary or more recently blood ketone concentrations is an integral part of self-management of type 1 diabetes, especially during acute illness, intermittent fasting, and religious fasts to prevent diabetic ketoacidosis. 163 Many people with type 1 diabetes do not adhere to urine or blood ketone testing, which likely results in unnecessary episodes of diabetic ketoacidosis. 164 Noting that blood and urine ketone testing is not widely available in all countries and settings is important. 1 Regular assessment of patients’ access to ketone testing (blood or urine) is critical for all clinicians. Euglycemic diabetic ketoacidosis in type 1 diabetes is a particular problem with concomitant use of SGLT-2 inhibitors; for this reason, these agents are not approved for use in these patients. For sick day management (and possibly for the future use of SGLT-2 inhibitors in people with type 1 diabetes), it is hoped that continuous ketone monitoring (CKM) can mitigate the risks of diabetic ketoacidosis. 165 Like CGM, the initial CKM device measures interstitial fluid β-hydroxybutyrate instead of glucose. CKM use becomes important in conjunction with a hybrid closed loop insulin pump system and added SGLT-2 inhibitor therapy, where insulin interruptions are common and hyperketonemia is frequent. 166
Perhaps the greatest technological challenge to date has been the development of non-invasive glucose monitoring. Numerous attempts have been made using strategies including optics, microwave, and electrochemistry. 167 Lack of success to date has resulted in healthy skepticism from the medical community. 168 However, active interest in the development of non-invasive technology with either interstitial or blood glucose remains.
Insulin and delivery systems
In the immediate future, two weekly basal insulins, insulin icodec and basal insulin Fc, may become available. 169 Studies of insulin icodec in type 1 diabetes are ongoing (ONWARDS 6; NCT04848480 ). How these insulins will be incorporated in management of type 1 diabetes is not yet clear.
Currently available AID systems use only a single hormone, insulin. Dual hormone AID systems incorporating glucagon are in development. 170 171 Barriers to the use of dual hormone systems include the need for a second chamber in the pump, a lack of stable glucagon formulations approved for long term subcutaneous delivery, lack of demonstrated long term safety, and gastrointestinal side effects from glucagon use. 74 Similarly, co-formulations of insulin and amylin (a hormone co-secreted with insulin and deficient in people with type 1 diabetes) are in development. 172
Immunotherapy for type 1 diabetes
As our understanding of the immunology of type 1 diabetes expands, development of the next generation of immunotherapies is under active pursuit. Antigen specific therapies, peptide immunotherapy, immune tolerance using DNA vaccination, and regulatory T cell based adoptive transfer targeting β cell senescence are all future opportunities for drug development. Combining immunotherapies with metabolic therapies such as GLP-1 receptor agonists to help to improve β cell mass is being actively investigated.
The quest for β cell replacement methods is ongoing. Transplantation of stem cell derived islets offers promise for personalized regenerative therapies as a potentially curative method that does away with the need for donor tissue. Since the first in vivo model of glucose responsive β cells derived from human embryonic stem cells, 173 different approaches have been attempted. Mesenchymal stromal cell treatment and autologous hematopoietic stem cells in newly diagnosed type 1 diabetes may preserve β cell function without any safety signals. 174 175 176 Stem cell transplantation for type 1 diabetes remains investigational. Encapsulation, in which β cells are protected using a physical barrier to prevent immune attack and avoid lifelong immunosuppression, and gene therapy techniques using CRISPR technology also remain in early stages of investigation.
Until recently, no specific guidelines for management of type 1 diabetes existed and management guidance was combined with consensus statements developed for type 2 diabetes. Table 6 summarizes available guidance and statements from various societies. A consensus report for management of type 1 diabetes in adults by the ADA and European Association for the Study of Diabetes became available in 2021; it covers several topics of diagnosis and management of type 1 diabetes, including glucose monitoring, insulin therapy, and acute complications. Similarly, the National Institute for Health and Care Excellence also offers guidance on management of various aspects of type 1 diabetes. Consensus statements for use of CGM, insulin pump, and AID systems are also available.
Guidelines in type 1 diabetes
Conclusions
Type 1 diabetes is a complex chronic condition with increasing worldwide prevalence affecting several million people. Several successes in management of type 1 diabetes have occurred over the years from the serendipitous discovery of insulin in 1921 to blood glucose monitoring, insulin pumps, transplantation, and immunomodulation. The past two decades have seen advancements in diagnosis, treatment, and technology including development of analog insulins, CGM, and advanced insulin delivery systems. Although we have gained a broad understanding on many important aspects of type 1 diabetes, gaps still exist. Pivotal research continues targeting immune targets to prevent or delay onset of type 1 diabetes. Although insulin is likely the oldest of existing modern drugs, no low priced generic supply of insulin exists anywhere in the world. Management of type 1 diabetes in under resourced areas continues to be a multifaceted problem with social, cultural, and political barriers.
Glossary of abbreviations
ADA—American Diabetes Association
AID—automated insulin delivery
BGM—blood glucose monitoring
CGM—continuous glucose monitoring
CKM—continuous ketone monitoring
DCCT—Diabetes Control and Complications Trial
DIY—do-it-yourself
FDA—Food and Drug Administration
GADA—glutamic acid decarboxylase antibody
GLP-1—glucagon-like peptide 1
GRS—genetic risk scoring
HbA1c—glycated hemoglobin
HCL—hybrid closed loop
LADA—latent autoimmune diabetes of adults
LMIC—low and middle income country
PAKT—pancreas after kidney transplant
RCT—randomized controlled trial
SGLT-2—sodium-glucose cotransporter 2
SPKT—simultaneous pancreas-kidney transplant
Questions for future research
What future new technologies can be helpful in management of type 1 diabetes?
How can newer insulin delivery methods benefit people with type 1 diabetes?
What is the role of disease modifying treatments in prevention and delay of type 1 diabetes?
Is there a role for sodium-glucose co-transporter inhibitors or glucagon-like peptide 1 receptor angonists in the management of type 1 diabetes?
As the population with type 1 diabetes ages, how should management of these people be tailored?
How can we better serve people with type 1 diabetes who live in under-resourced settings with limited access to medications and technology?
How patients were involved in the creation of this manuscript
A person with lived experience of type 1 diabetes reviewed a draft of the manuscript and offered input on important aspects of their experience that should be included. This person is involved in large scale education and activism around type 1 diabetes. They offered their views on various aspects of type 1 diabetes, especially the use of adjuvant therapies and the burden of living with diabetes. This person also raised the importance of education of general practitioners on the various stages of type 1 diabetes and the management aspects. On the basis of this feedback, we have highlighted the burden of living with diabetes on a daily basis.
Series explanation: State of the Art Reviews are commissioned on the basis of their relevance to academics and specialists in the US and internationally. For this reason they are written predominantly by US authors
Contributors: SS and IBH contributed to the planning, drafting, and critical review of this manuscript. FNK contributed to the drafting of portions of the manuscript. All three authors are responsible for the overall content as guarantors.
Competing interests: We have read and understood the BMJ policy on declaration of interests and declare the following interests: SS has received an honorarium from Abbott Diabetes Care; IBH has received honorariums from Abbott Diabetes Care, Lifescan, embecta, and Hagar and research support from Dexcom and Insulet.
Provenance and peer review: Commissioned; externally peer reviewed.
- DeVries JH ,
- Hess-Fischl A ,
- Gregory GA ,
- Robinson TIG ,
- Linklater SE ,
- International Diabetes Federation Diabetes Atlas Type 1 Diabetes in Adults Special Interest Group
- Harding JL ,
- Wander PL ,
- Dabelea D ,
- Mayer-Davis EJ ,
- SEARCH for Diabetes in Youth Study
- Lawrence JM ,
- SEARCH for Diabetes in Youth Study Group
- Fazeli Farsani S ,
- Souverein PC ,
- van der Vorst MM ,
- Sutherland J ,
- Rokszin G ,
- Stahl-Pehe A ,
- Kamrath C ,
- Atkinson MA ,
- Bingley PJ ,
- Bonifacio E ,
- Leslie RD ,
- Evans-Molina C ,
- Freund-Brown J ,
- Thomas NJ ,
- Zimmet PZ ,
- Rowley MJ ,
- Knowles W ,
- Fourlanos S ,
- Greenbaum CJ ,
- ElSayed NA ,
- American Diabetes Association
- Miller RG ,
- Secrest AM ,
- Sharma RK ,
- Songer TJ ,
- McDonald T ,
- Greenfield JR
- Tridgell DM ,
- Spiekerman C ,
- Greenbaum CJ
- Glessner J ,
- Foster NC ,
- Miller KM ,
- Becker DJ ,
- Khawandanah J
- Pedrosa MR ,
- Franco DR ,
- Gieremek HW ,
- Nathan DM ,
- Diabetes Control and Complications Trial Research Group
- Klonoff DC ,
- Parkes JL ,
- Kovatchev BP ,
- Raghinaru D ,
- iDCL Trial Research Group
- Riddlesworth T ,
- DIAMOND Study Group
- Leelarathna L ,
- Neupane S ,
- FLASH-UK Trial Study Group
- Polonsky W ,
- Hirsch IB ,
- Pratley RE ,
- Kanapka LG ,
- Rickels MR ,
- Wireless Innovation for Seniors With Diabetes Mellitus (WISDM) Study Group
- Tauschmann M ,
- APCam11 Consortium
- Russell SJ ,
- Damiano ER ,
- Bionic Pancreas Research Group
- Bailey TS ,
- Group Information ,
- Bergenstal RM ,
- Dellva MA ,
- Mathieu C ,
- Herold KC ,
- Type 1 Diabetes TrialNet Study Group
- Libman IM ,
- DiMeglio LA ,
- T1D Exchange Clinic Network Metformin RCT Study Group
- Petrie JR ,
- Chaturvedi N ,
- REMOVAL Study Group
- Dandona P ,
- Phillip M ,
- DEPICT-1 Investigators
- Rosenstock J ,
- Marquard J ,
- Laffel LM ,
- Hemmingsson JU ,
- ADJUNCT ONE Investigators
- Pieber TR ,
- ADJUNCT TWO Investigators
- Reynolds J ,
- Battelino T ,
- Liljenquist D ,
- Becker RH ,
- Bergmann K ,
- Lehmann A ,
- Cheng AYY ,
- Stender-Petersen K ,
- Hövelmann U ,
- Carlson AL ,
- Komatsu M ,
- Coutant DE ,
- Stamati A ,
- Karagiannis T ,
- Christoforidis A
- Heinemann L ,
- Baughman R ,
- Akturk HK ,
- Snell-Bergeon JK ,
- Prabhu JN ,
- Seyed Ahmadi S ,
- Westman K ,
- Pivodic A ,
- Hermann JM ,
- Freiberg C ,
- DPV Initiative
- Dicembrini I ,
- Cosentino C ,
- Mannucci E ,
- Abelseth J ,
- Karageorgiou V ,
- Papaioannou TG ,
- Weisman A ,
- Cardinez M ,
- Kramer CK ,
- Asarani NAM ,
- Reynolds AN ,
- Elbalshy M ,
- Jennings P ,
- Burnside MJ ,
- Williman JA ,
- Fridell JA ,
- Stratta RJ ,
- Gruessner AC
- Robertson RP
- Shapiro AM ,
- Pepper AR ,
- Shapiro AMJ
- Walker JT ,
- Saunders DC ,
- Brissova M ,
- Gitelman SE ,
- Bluestone JA
- Hagopian W ,
- Ferry RJ Jr . ,
- Protégé Trial Investigators
- von Scholten BJ ,
- Kreiner FF ,
- Gough SCL ,
- von Herrath M
- Type 1 Diabetes TrialNet Abatacept Study Group
- Hardie DG ,
- Dejgaard TF ,
- Christiansen E ,
- ADJUNCT ONE and ADJUNCT TWO Investigators
- Yunasan E ,
- Peters AL ,
- Palanca A ,
- van Nes F ,
- Ampudia Blasco FJ ,
- Dobbins RL ,
- Greenway FL ,
- Zambrowicz BP ,
- Brodovicz K ,
- Soleymanlou N ,
- Wissinger E ,
- Juhaeri J ,
- Mayer-Davis EJ
- Dhatariya KK ,
- Glaser NS ,
- Umpierrez GE
- Ramphul K ,
- Umpierrez G ,
- Korytkowski M
- Weinstock RS ,
- T1D Exchange Clinic Network
- Eshkoli T ,
- Brandstaetter E ,
- Jotkowitz A
- Dhatariya KK
- Joint British Diabetes Societies for Inpatient Care
- Kilpatrick ES ,
- Butler AE ,
- Ostlundh L ,
- Koufakis T ,
- Agiostratidou G ,
- International Hypoglycaemia Study Group
- van de Ven KC ,
- Heerschap A ,
- van der Graaf M ,
- de Galan BE
- Alsifri S ,
- Aronson R ,
- HAT Investigator Group
- Pettus JH ,
- Shepherd L ,
- Van Houten HK ,
- Ziegenfuss JY ,
- Wermers RA ,
- Schernthaner G ,
- Anderson J ,
- Saunders AL ,
- Snell-Bergeon J ,
- Forlenza GP ,
- Bispham J ,
- Gabbay RA ,
- Pontiroli AE ,
- Tagliabue E
- T1D Exchange Intranasal Glucagon Investigators
- Freckmann G ,
- Ehrmann D ,
- El Laboudi A ,
- Spanudakis E ,
- Anantharaja S ,
- Peleckis AJ ,
- Dalton-Bakes C ,
- van Beers CA ,
- Kleijer SJ ,
- CGM Intervention in Teens and Young Adults with T1D (CITY) Study Group ,
- Piras de Oliveira C ,
- Ribeiro A ,
- Chigutsa F ,
- Malecki MT ,
- Hopkins D ,
- Lawrence I ,
- Mansell P ,
- Stanton-Fay SH ,
- Hamilton K ,
- Chadwick PM ,
- DAFNEplus study group
- Goldsmith K ,
- Yudkin JS ,
- Buntinx F ,
- Mapatano MA ,
- De Clerck M ,
- Truyers C ,
- Chambers D ,
- O’Cathain A
- Klatman EL ,
- Auzanneau M ,
- Tanenbaum ML ,
- Iturralde E ,
- Lipman TH ,
- Bhutta ZA ,
- Pfiester E ,
- Thieffry A ,
- Ballhausen H ,
- Gajewska KA ,
- O’Donnell S
- Wareham NJ ,
- Joosse HJ ,
- Raposo JF ,
- de Courten M
- Hemmingsen B ,
- Abouhassan T ,
- Albanese-O’Neill A ,
- Jacobsen L ,
- Haller MJ ,
- Castorino K ,
- Lovblom LE ,
- Cardinez N ,
- Nguyen KT ,
- Andersen G ,
- Meiffren G ,
- Famulla S ,
- Castellanos LE ,
- Balliro CA ,
- Sherwood JS ,
- Tsoukas MA ,
- Bernier-Twardy S ,
- Martinson LA ,
- Carlsson PO ,
- Schwarcz E ,
- Korsgren O ,
- Oliveira MC ,
- Stracieri AB ,
- Buzzetti R ,
- Mauricio D ,
- McGibbon A ,
- Ingersoll K ,
- Tugwell B ,
- Diabetes Canada Clinical Practice Guidelines Expert Committee
- Fleming GA ,
- McCall AL ,
- Gianchandani R ,
- Skip to main content
- Skip to FDA Search
- Skip to in this section menu
- Skip to footer links

The .gov means it’s official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you're on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
U.S. Food and Drug Administration
- Search
- Menu
- News & Events
- FDA Newsroom
- Press Announcements
FDA Approves First Cellular Therapy to Treat Patients with Type 1 Diabetes
FDA News Release
Today, the U.S. Food and Drug Administration approved Lantidra, the first allogeneic (donor) pancreatic islet cellular therapy made from deceased donor pancreatic cells for the treatment of type 1 diabetes. Lantidra is approved for the treatment of adults with type 1 diabetes who are unable to approach target glycated hemoglobin (average blood glucose levels) because of current repeated episodes of severe hypoglycemia (low blood sugar) despite intensive diabetes management and education.
“Severe hypoglycemia is a dangerous condition that can lead to injuries resulting from loss of consciousness or seizures,” said Peter Marks, M.D., Ph.D., director of the FDA’s Center for Biologics Evaluation and Research. “Today’s approval, the first-ever cell therapy to treat patients with type 1 diabetes, provides individuals living with type 1 diabetes and recurrent severe hypoglycemia an additional treatment option to help achieve target blood glucose levels.”
Type 1 diabetes is a chronic autoimmune disease that requires lifelong care including requiring insulin, either through multiple daily injections or continuous infusion using a pump, every day to live. People with type 1 diabetes also perform blood glucose checks several times a day to guide the management of their diabetes.
Some people with type 1 diabetes have trouble managing the amount of insulin needed every day to prevent hyperglycemia (high blood sugar) without causing hypoglycemia. They may also develop hypoglycemia unawareness, where they are unable to detect their blood glucose is dropping and may not have a chance to treat themselves to prevent their blood glucose from further dropping. This makes it difficult to dose insulin. Lantidra provides a potential treatment option for these patients.
The primary mechanism of action of Lantidra is believed to be the secretion of insulin by the infused allogeneic islet beta cells. In some patients with type 1 diabetes, these infused cells can produce enough insulin, so the patient no longer needs to take insulin (by injections or pump) to control their blood sugar levels. Lantidra is administered as a single infusion into the hepatic (liver) portal vein. An additional infusion of Lantidra may be performed depending on the patient’s response to the initial dose.
The safety and effectiveness of Lantidra was evaluated in two non-randomized, single-arm studies in which a total of 30 participants with type 1 diabetes and hypoglycemic unawareness received at least one infusion and a maximum of three infusions. Overall, 21 participants did not need to take insulin for a year or more, with 11 participants not needing insulin for one to five years and 10 participants not needing insulin for more than five years. Five participants did not achieve any days of insulin independence.
Adverse reactions associated with Lantidra varied with each participant depending on the number of infusions they received and the length of time they were followed and may not reflect the rates observed in practice The most common adverse reactions included nausea, fatigue, anemia, diarrhea and abdominal pain. A majority of participants experienced at least one serious adverse reaction related to the procedure for infusing Lantidra into the hepatic portal vein and the use of immunosuppressive medications needed to maintain the islet cell viability. Some serious adverse reactions required discontinuation of immunosuppressive medications, which resulted in the loss of islet cell function and insulin independence. These adverse events should be considered when assessing the benefits and risks of Lantidra for each patient. Lantidra is approved with patient-directed labeling to inform patients with type 1 diabetes about benefits and risks of Lantidra.
The FDA granted approval of Lantidra to CellTrans Inc.
The FDA, an agency within the U.S. Department of Health and Human Services, protects the public health by assuring the safety, effectiveness, and security of human and veterinary drugs, vaccines and other biological products for human use, and medical devices. The agency also is responsible for the safety and security of our nation’s food supply, cosmetics, dietary supplements, products that give off electronic radiation, and for regulating tobacco products.
Thank you for visiting nature.com. You are using a browser version with limited support for CSS. To obtain the best experience, we recommend you use a more up to date browser (or turn off compatibility mode in Internet Explorer). In the meantime, to ensure continued support, we are displaying the site without styles and JavaScript.
- View all journals
- Explore content
- About the journal
- Publish with us
- Sign up for alerts
Type 1 diabetes articles within Nature Reviews Endocrinology
Review Article | 03 September 2024
Harnessing cellular therapeutics for type 1 diabetes mellitus: progress, challenges, and the road ahead
Type 1 diabetes mellitus affects 8.5 million people globally and is characterized by autoimmune destruction of pancreatic β cells. This Review discusses cell replacement therapies for T1DM and outlines the challenges and future directions
- Alessandro Grattoni
- , Gregory Korbutt
- & Paul de Vos
Research Highlight | 02 August 2024
Combination therapy increases human β-cell mass in vivo
- Olivia Tysoe
Review Article | 18 June 2024
The relationship between SARS-CoV-2 infection and type 1 diabetes mellitus
Many studies identified an increase in the incidence of type 1 diabetes mellitus (T1DM) during the COVID-19 pandemic, but other reports do not support this association. This Review addresses the issue of the involvement of SARS-CoV-2 infection in the development of T1DM using evidence from epidemiological, clinical and experimental studies.
- Cyril Debuysschere
- , Magloire Pandoua Nekoua
- & Didier Hober
Correspondence | 21 March 2024
Reply to ‘Slowly progressive insulin dependent diabetes mellitus in type 1 diabetes endotype 2’
- Maria J. Redondo
- & Noel G. Morgan
Slowly progressive insulin-dependent diabetes mellitus in type 1 diabetes endotype 2
- Tetsuro Kobayashi
- & Takashi Kadowaki
Year in Review | 06 December 2023
Type 1 diabetes mellitus: a brave new world
One hundred years after the Nobel prize was bestowed on Banting and McLeod for the ‘discovery’ of insulin, we are again seeing major evolutions in the management of type 1 diabetes mellitus, with the prospect of achieving disease control beyond mere management now becoming real. Here, we discuss the latest, most notable developments.
- Pieter-Jan Martens
- & Chantal Mathieu
Research Highlight | 24 November 2023
β-cells protected from T1DM by early senescence programme
Research Highlight | 26 October 2023
Antivirals in the treatment of new-onset T1DM
- Claire Greenhill
Review Article | 19 June 2023
Heterogeneity and endotypes in type 1 diabetes mellitus
There is a growing awareness that type 1 diabetes mellitus (T1DM) is a heterogeneous disease that can be characterized into distinct endotypes. This Review discusses the evidence for endotypes in T1DM and explores the implications for clinical practice.
Research Highlight | 07 June 2023
Differences in stem cell-derived islets
Perspective | 22 May 2023
Insulin detection in diabetes mellitus: challenges and new prospects
An urgent need exists for technologies and devices capable of frequent and real-time insulin measurements in patients with diabetes mellitus to guide optimal insulin dosing. This Perspective discusses the advances and challenges in moving insulin assays from laboratory-based assays to frequent and continuous measurements in decentralized settings.
- , Ponnusamy Nandhakumar
- & Joseph Wang
Clinical Outlook | 18 May 2023
Approval of teplizumab: implications for patients
Type 1 diabetes mellitus (T1DM) can be predicted, and immune therapy can alter the progression of the disease. The FDA’s approval of teplizumab as the first disease-modifying therapy for T1DM and the first therapy aimed at delaying the clinical onset of any immune-mediated disease represents a paradigm shift in the treatment of T1DM.
- Cate Speake
- & Carla J. Greenbaum
Perspective | 18 April 2023
Why does the immune system destroy pancreatic β-cells but not α-cells in type 1 diabetes?
In type 1 diabetes, the immune system destroys pancreatic β-cells but not neighbouring α-cells. Here, the authors describe the key differences between β-cells and α-cells that could account for their differential autoimmune vulnerability, and how these differences could result in the preferential endurance and survival of α-cells over β-cells.
- Decio L. Eizirik
- , Florian Szymczak
- & Roberto Mallone
Perspective | 13 March 2023
A perspective on treating type 1 diabetes mellitus before insulin is needed
This Perspective discusses potential approaches to managing patients in the early stages of developing type 1 diabetes mellitus, which could enable the initiation of insulin therapy to be delayed in some patients.
- Danijela Tatovic
- , Parth Narendran
- & Colin M. Dayan
Research Highlight | 10 March 2023
Interventions in people newly diagnosed with type 1 diabetes mellitus
Research Highlight | 24 February 2023
Reprogramming lymph nodes in type 1 diabetes mellitus
- Shimona Starling
News & Views | 04 January 2023
Monogenic diabetes mellitus hidden in autoantibody-negative diabetes mellitus
A considerable proportion of autoantibody-negative children with type 1 diabetes mellitus actually have monogenic forms of diabetes mellitus, which enables tailored treatment. Thus, a diagnosis of monogenic diabetes mellitus should be considered and genetically tested for in this group of patients, even if the clinical criteria for monogenic diabetes mellitus are not met.
- Stepanka Pruhova
- & Petra Dusatkova
Research Highlight | 31 October 2022
Engineered T regs prevent diabetes mellitus in mice
Review Article | 31 October 2022
Exercise in adults with type 1 diabetes mellitus
Exercise has many beneficial effects; however, glycaemia needs to be carefully managed in patients with type 1 diabetes mellitus undertaking exercise. This Review characterizes the exercise response in people with type 1 diabetes mellitus and provides clinical management strategies to address glucose control around exercise.
- Michael C. Riddell
- & Anne L. Peters
Hypoglycaemia in type 1 diabetes mellitus: risks and practical prevention strategies
Hypoglycaemia is a common occurrence in people with type 1 diabetes mellitus, and can have serious consequences. This Review defines hypoglycaemia in type 1 diabetes mellitus, and also outlines its frequency, risk factors and adverse outcomes. Ways to prevent and treat this complication of insulin therapy are also discussed.
- Jasleen Kaur
- & Elizabeth R. Seaquist
In Brief | 09 September 2022
Cognitive function in T1DM improved by hybrid closed-loop insulin delivery
News & Views | 15 August 2022
Glucagon receptor antagonists might stimulate β-cell expansion
In a recent issue of Cell Reports , Xi et al. reported on their studies of an anti-glucagon receptor antibody in several mouse models of insulin-deficient diabetes mellitus, in which they show substantial increase in β-cell mass from enhanced replication and transdifferentiation of glucagon-expressing α-cells to insulin-expressing β-cells.
- Maria F. Rubin de Celis
- & Susan Bonner-Weir
Research Highlight | 26 July 2022
Highlights from ADA 82 nd Scientific Sessions
Review Article | 06 June 2022
The burden and risks of emerging complications of diabetes mellitus
This article discusses evidence for the emergence of a different set of complications associated with diabetes mellitus from the traditional ones, outlines the risks and burden of these associated complications and considers implications for the future management of diabetes mellitus.
- Dunya Tomic
- , Jonathan E. Shaw
- & Dianna J. Magliano
Review Article | 01 June 2022
Persistent coxsackievirus B infection and pathogenesis of type 1 diabetes mellitus
This Review highlights evidence that persistent enterovirus infections, particularly coxsackievirus B, trigger and/or accelerate islet autoimmunity in susceptible individuals, thereby leading to type 1 diabetes mellitus (T1DM). The potential for vaccination or antiviral therapies to prevent T1DM onset is also considered.
- Magloire Pandoua Nekoua
- , Enagnon Kazali Alidjinou
Comment | 16 May 2022
Progress in islet transplantation is more important than ever
It is increasingly clear that pancreatic islet replacement is needed to provide a comprehensive treatment for the growing numbers of patients with type 1 diabetes mellitus. Advances from the past year suggest that this goal might now be within reach.
- Stefan R. Bornstein
- , Barbara Ludwig
- & Charlotte Steenblock
Research Highlight | 20 April 2022
GLP1–oestrogen agonist protects β-cells from insulin-deficient diabetes mellitus
In Brief | 08 March 2022
Multi-omics analyses of human islets in T1DM
Research Highlight | 23 February 2022
Increasing success of islet transplantation
Research Highlight | 10 December 2021
Stem-cell derived pancreatic endoderm cells in the treatment of T1DM
Research Highlight | 08 December 2021
Exploring the regulation of glucagon secretion
In Brief | 25 October 2021
Potential role for follicular T reg cells in T1DM
Research Highlight | 05 October 2021
Melatonin prevents diabetes mellitus-induced bone loss
Comment | 24 September 2021
Type 1 diabetes mellitus and polycystic ovary syndrome
Up to one in four women with type 1 diabetes mellitus (T1DM) also have polycystic ovary syndrome (PCOS). Under subcutaneous insulin administration, systemic hyperinsulinism might trigger PCOS in women predisposed to the condition. However, very little is known about the long-term consequences of androgen excess in women with T1DM, and management guidelines are lacking.
- Héctor F. Escobar-Morreale
- , Ane Bayona
- & Manuel Luque-Ramírez
Review Article | 17 August 2021
One hundred years of insulin therapy
It is 100 years since the famous experiments that identified insulin and showed that this protein could be used to treat people with type 1 diabetes mellitus. This Review charts the developments in insulin research over the past century and highlights future directions for this field.
- Chantal Mathieu
- , Pieter-Jan Martens
- & Roman Vangoitsenhoven
In Brief | 30 June 2021
The largest study of genetics of T1DM
News & Views | 24 June 2021
Temporal coding of ERK signalling in β-cells
A new study has reported genetic evidence that MEK–ERK signalling is needed by β-cells, both for maintenance of β-cell mass and for optimization of insulin release. Their results point towards a new challenge of disentangling ERK signalling across multiple time scales.
- Mark O. Huising
- & John G. Albeck
Research Highlight | 22 March 2021
New combination therapy shows promise for recent-onset type 1 diabetes mellitus
Review Article | 08 December 2020
Type 1 diabetes mellitus as a disease of the β-cell (do not blame the immune system?)
This Review examines the evidence that β-cells are active participants in the dialogue with the immune system during the development of type 1 diabetes mellitus. The authors suggest that therapies targeting β-cell health, vitality and function might prove essential, in combination with immunotherapy, to change the course of events leading to β-cell destruction.
- Bart O. Roep
- , Sofia Thomaidou
- & Arnaud Zaldumbide
Year in Review | 30 November 2020
Shortening the paths to type 1 diabetes mellitus prevention
The development and application of effective immunotherapies for type 1 diabetes mellitus has lagged behind our ability to identify and stage individuals in pre-clinical stages of disease. This Year in Review addresses advances in immunotherapy aimed towards prevention and our readiness to roll out screening in the broader population.
- Anette-G. Ziegler
- & Ezio Bonifacio
News & Views | 21 October 2020
Transplantation of stem cell-derived pancreatic islet cells
A large fraction of patients with diabetes mellitus require insulin treatment to control glucose metabolism; however, this treatment brings risks of hypoglycaemia and provides suboptimal metabolic control. Transplantation of stem cell-derived pancreatic islet cells could be an ideal solution, which is approaching clinical translation.
- Giacomo Lanzoni
- & Camillo Ricordi
Research Highlight | 02 September 2020
Type 1 diabetes mellitus: another step closer to pancreatic β-cell transplantation
- Alan Morris
Comment | 28 August 2020
Revisiting the role of inflammation in the loss of pancreatic β-cells in T1DM
Islet inflammation (insulitis) in type 1 diabetes mellitus is triggered by a deleterious dialogue between β-cells and the immune system, inducing β-cell dysfunction and death. This concept, outlined in our 2009 Review, has been confirmed and extended. Here, we provide a brief update of the field and outline key pending questions.
- & Maikel L. Colli
News & Views | 14 July 2020
A novel cellular engineering approach to diabetes mellitus
For type 1 diabetes mellitus (T1DM), keeping glucose levels within the normal range of 65–150 mg/dl with administered insulin has had limited success. Now, Fussenegger and colleagues have engineered cells to release insulin in response to electrical signals, but can this advance lead to better glucose control?
- Gordon C. Weir
Review Article | 25 June 2020
Emerging routes to the generation of functional β-cells for diabetes mellitus cell therapy
This Review highlights the research advances, advantages and challenges in several different strategies for generating functional β-cells for therapeutic use in diabetes mellitus. In addition, scalable bioengineering processes are also discussed for the realization of the therapeutic potential of derived β-cells.
- Gopika G. Nair
- , Emmanuel S. Tzanakakis
- & Matthias Hebrok
Review Article | 12 May 2020
Pancreatic β-cells in type 1 and type 2 diabetes mellitus: different pathways to failure
Understanding the mechanisms behind β-cell failure in diabetes mellitus is critical to prevent or revert disease. This Review highlights new findings from studies performed on human β-cells or on samples obtained from patients with type 1 or type 2 diabetes mellitus.
- Décio L. Eizirik
- , Lorenzo Pasquali
- & Miriam Cnop
Research Highlight | 01 May 2020
Role of long non-coding RNA in T1DM
Research Highlight | 07 April 2020
β-cell dedifferentiation prior to insulitis prevents T1DM
Research Highlight | 09 March 2020
Restoring β-cells
News & Views | 12 February 2020
A predictive CD8 + T cell phenotype for T1DM progression
In a cross-sectional study of individuals with type 1 diabetes mellitus, those who were designated to be slow disease progressors had an increased proportion of autoreactive, islet-specific CD8 + T cells expressing an ‘exhausted’ phenotype. By contrast, rapid disease progressors had increased numbers of islet-specific CD8 + T cells with a transitional memory phenotype.
- F. Susan Wong
- & Li Wen
Browse broader subjects
- Autoimmune diseases
Quick links
- Explore articles by subject
- Guide to authors
- Editorial policies
- My Events / Fundraisers
- Monthly Giving
- Vehicle Donation
- Workplace Giving
- Find a Fundraiser
- Ways to Fundraise
We are Breakthrough T1D
We’re here to make every day with type 1 diabetes better, and we won’t stop until the condition is a thing of the past.

Get resources + support
As we drive toward curing type 1 diabetes (T1D), we help make everyday life better for the people who face it.

Learn about the symptoms of type 1 diabetes and get answers to common questions about the condition

Newly diagnosed
Get the support and information you need to understand and manage type 1 diabetes

Life with T1D
What you need to know about navigating life with type 1 diabetes at all ages and stages

T1D management
Learn about checking blood sugar, administering insulin, counting carbs, and more

Breakthrough T1D is the leading global type 1 diabetes research and advocacy organization.
Get involved.
Advocate. Engage. Inspire. Participate. Volunteer. Help us accelerate breakthroughs for T1D!

Connect with the community
Connect with a supportive local + global T1D community
Power the movement
We’re creating a movement for the entire T1D community

Accelerating T1D breakthroughs
This is more than a moment—we’re creating a movement. We connect the brightest minds to help advance treatments, influence policy, and improve access to care for those all over the world who need it. Today, we are leading the way to more effective solutions. Tomorrow, we will make this condition a thing of the past.
Breakthrough T1D news + updates
T1D information and developments you need to know
Veronica Beard Gives Back to Breakthrough T1D
Navigating the school year with type 1 diabetes: A call to support and action

Strength, struggle, and resilience: my mom’s journey with T1D
Be the first to know about t1d news, events and more.
Sign up to receive updates from Breakthrough T1D
- First name *
- Last name *
- Comments This field is for validation purposes and should be left unchanged.
Join the movement to end T1D
Champion federal funding for T1D research. Inform health and regulatory policy. Improve lives.

Your privacy
We value your privacy. When you visit BreakthroughT1D.org (and our family of websites), we use cookies to process your personal data in order to customize content and improve your site experience, provide social media features, analyze our traffic, and personalize advertising. By choosing “I Agree”, you understand and agree to Breakthrough T1D's Privacy Policy
- Español ( Spanish )

Study provides preliminary evidence in favor of a new type 1 diabetes treatment

Type 1 diabetes is an autoimmune disease that causes the body's immune system to attack and destroy insulin-producing beta cells in the pancreas. Traditional management of type 1 diabetes has primarily involved replacing the missing insulin with injections which, though effective, can be expensive and burdensome. A new study led by researchers at the University of Chicago Medicine and Indiana University suggests that an existing drug could be repurposed to treat type 1 diabetes, potentially reducing dependence on insulin as the sole treatment.
The research centers on a medication known as α-difluoromethylornithine (DFMO), which inhibits an enzyme that plays a key role in cellular metabolism. The latest translational results are a culmination of years of research: In 2010, while corresponding author Raghu Mirmira, MD, PhD , was at Indiana University, he and his lab performed fundamental biochemistry experiments on beta cells in culture. They found that suppressing the metabolic pathway altered by DFMO helped protect the beta cells from environmental factors, hinting at the possibility of preserving and even restoring these vital cells in patients diagnosed with type 1 diabetes.
The researchers confirmed their observations preclinically in zebrafish and then in mice before senior author Linda DiMeglio, MD, MPH, Edwin Letzter Professor of Pediatrics at Indiana University School of Medicine and a pediatric endocrinologist at Riley Children's Health, launched a clinical trial to evaluate the safety and tolerability of the drug in type 1 diabetes patients. The results of the trial, which was funded by the Juvenile Diabetes Research Foundation (JDRF) and used DMFO provided by Panbela Therapeutics, indicated that the drug is safe for type 1 diabetes patients and can help keep insulin levels stable by protecting beta cells.
“As a physician-scientist, this is the kind of thing we’ve always strived for – to discover something at a very basic, fundamental level in cells and find a way to bring it into the clinic,” said Mirmira, who is now Professor of Medicine and an endocrinologist at UChicago Medicine. “It definitely underscores the importance of supporting basic science research.”
"It's been truly thrilling to witness the promising results in the pilot trial after this long journey, and we're excited to continue our meaningful collaboration," said DiMeglio.
Importantly, DFMO has already been FDA-approved as a high dose injection since 1990 for treating African Sleeping Sickness and received breakthrough therapy designation for neuroblastoma maintenance therapy after remission in 2020. Pre-existing regulatory approval could potentially facilitate its use in type 1 diabetes, saving effort and expense and getting the treatment to patients sooner.
“For a drug that’s already approved for other indications, the approval timeline can be a matter of years instead of decades once you have solid clinical evidence for safety and efficacy,” said Mirmira. “Using a new formulation of DFMO as a pill allows patients to take it by mouth instead of needing to undergo regular injections, and it has a very favorable side effect profile. It’s exciting to say we have a drug that works differently from every other treatment we have for this disease.”
To follow up on the recently published results, first and co-corresponding author Emily K. Sims, MD, Associate Professor of Pediatrics at IU School of Medicine and a pediatric endocrinologist at Riley Children's Health, launched a multi-center clinical trial, also funded by JDRF – with UChicago among the trial sites – to gather even stronger data regarding the efficacy of DFMO as a type 1 diabetes treatment.
"With our promising early findings, we hold hope that DFMO, possibly as part of a combination therapy, could offer potential benefits to preserve insulin secretion in individuals with recent-onset type 1 diabetes and ultimately also be tested in those who are at risk of developing the condition," said Sims.
“A new era is dawning where we’re thinking of novel ways to modify the disease using different types of drugs and targets that we didn’t classically think of in type 1 diabetes treatment,” said Mirmira.
The study, “Inhibition of Polyamine Biosynthesis Preserves β-Cell Function in Type 1 Diabetes,” was published in Cell Medicine Reports in November 2023. Co-authors include Emily K. Sims, Abhishek Kulkarni, Audrey Hull, Stephanie E. Woerner, Susanne Cabrera, Lucy D. Mastrandrea, Batoul Hammoud, Soumyadeep Sarkar, Ernesto S. Nakayasu, Teresa L. Mastracci, Susan M. Perkins, Fangqian Ouyang, Bobbie-Jo Webb-Robertson, Jacob R. Enriquez, Sarah A. Tersey, Carmella Evans-Molina, S. Alice Long, Lori Blanchfield, Eugene W. Gerner, Raghavendra Mirmira, and Linda A. DiMeglio.
- Utility Menu
GA4 tracking code

A new therapy for treating Type 1 diabetes
Promising early results show that longstanding harvard stem cell institute (hsci) research may have paved the way for a breakthrough treatment of type 1 diabetes. utilizing research from the melton lab, vertex pharmaceuticals has developed vx-880, an investigational stem cell-derived, fully differentiated pancreatic islet cell replacement therapy for people with type 1 diabetes (t1d). in conjunction with immunosuppressive therapy, vx-880 produced robust restoration of islet cell function on day 90 in the first patient in its phase 1/2 clinical trial..

The patient was treated with a single infusion of VX-880 at half the target dose in conjunction with immunosuppressive therapy. The patient, who was diagnosed with T1D 40 years ago and has been dependent on exogenous (injected) insulin, achieved successful engraftment and demonstrated rapid and robust improvements in multiple measures. These included increases in fasting and stimulated C-peptide, improvements in glycemic control, including HbA1c, and decreases in exogenous insulin requirement, signifying the restoration of insulin-producing islet cells.
VX-880 is not only a potential breakthrough in the treatment of T1D, it is also one of the very first demonstrations of the practical application of embryonic stem cells, using stem cells that have been differentiated into functional islets to treat a patient, explained Doug Melton, Ph.D., co-director of HSCI, is the Xander University Professor at Harvard and an Investigator of the Howard Hughes Medical Institute. Unlike prior treatments, this innovative therapy gives the patient functional hormone producing cells that control glucose metabolism. This potentially obviates the lifelong need for patients with diabetes to self-inject insulin as the replacement cells “provide the patient with the natural factory to make their own insulin,” explained Melton.
These results from the first patient treated with VX-880 are unprecedented. What makes these results truly remarkable is that they were achieved with only half the target dose,” said Bastiano Sanna, Ph.D., Executive Vice President and Chief of Cell and Genetic Therapies at Vertex. “While still early, these results support the continued progression of our VX-880 clinical studies, as well as future studies using our encapsulated islet cells, which hold the potential to be used without the need for immunosuppression.”
“As a surgeon who has worked in the field of islet cell transplantation for decades, this approach, which obviates the need for an organ donor, could be a game changer,” said James Markmann, M.D., Ph.D., Professor of Surgery and Chief of the Division of Transplant Surgery at Massachusetts General Hospital. “We are excited to progress this unique and potentially transformative medicine through clinical trials and to patients.”
“More than a decade ago our lab had a vision for developing an islet cell replacement therapy to provide a functional cure to people suffering from T1D,” said Melton, a founder and one of the first co-chairs of the Harvard Stem Cell and Regenerative Biology Department. “These promising results bring great hope that stem cell-derived, fully differentiated islet cells could deliver a life-changing therapy for people who suffer from the relentless life-long burden of T1D. I'm so grateful that Harvard and the Harvard Stem Cell Institute have supported this work.”
Latest News
How a small fish could lead to better strategies to repair tendon tears, jason buenrostro lands macarthur ‘genius grant’, new model for in vitro production of human brown fat cells lays groundwork for obesity, diabetes cell therapy, share this story, news by topic.
- Alzheimer's Disease (8)
- Bioengineering (31)
- Blood Diseases (52)
- Cancer (55)
- Cardiovascular Disease (25)
- Diabetes (30)
- Endocrine Disease (1)
- Eye Diseases (10)
- Fibrosis (6)
- Gastrointestinal Disease (8)
- Genetics/Epigenetics (24)
- Graft-Versus-Host Disease (1)
- Hearing Loss (5)
- Immunology (15)
- Kidney Disease (12)
- Liver Disease (6)
- Lung Disease (9)
- Multiple Sclerosis (1)
- Biochemistry and Molecular Biology
- Biostatistics
- Environmental Health and Engineering
- Epidemiology
- Health Policy and Management
- Health, Behavior and Society
- International Health
- Mental Health
- Molecular Microbiology and Immunology
- Population, Family and Reproductive Health
- Program Finder
- Admissions Services
- Course Directory
- Academic Calendar
- Hybrid Campus
- Lecture Series
- Convocation
- Strategy and Development
- Implementation and Impact
- Integrity and Oversight
- In the School
- In the Field
- In Baltimore
- Resources for Practitioners
- Articles & News Releases
- In The News
- Statements & Announcements
- At a Glance
- Student Life
- Strategic Priorities
- Inclusion, Diversity, Anti-Racism, and Equity (IDARE)
- What is Public Health?
Research Gaps Around Type 1 Diabetes
A large body of research on Type 2 diabetes has helped to develop guidance, informing how patients are diagnosed, treated, and manage their lifestyle. In contrast, Type 1 diabetes, often mistakenly associated only with childhood, has received less attention.
In this Q&A, adapted from the April 17 episode of Public Health On Call , Stephanie Desmon speaks to Johns Hopkins epidemiologists Elizabeth Selvin , PhD '04, MPH, and Michael Fang , PhD, professor and assistant professor, respectively, in the Department of Epidemiology, about recent findings that challenge common beliefs about type 1 diabetes. Their conversation touches on the misconception that it’s solely a childhood condition, the rise of adult-onset cases linked to obesity, and the necessity for tailored approaches to diagnosis and care. They also discuss insulin prices and why further research is needed on medications like Ozempic in treating Type 1 diabetes.
I want to hear about some of your research that challenges what we have long understood about Type 1 diabetes, which is no longer called childhood diabetes.
MF: Type 1 diabetes was called juvenile diabetes for the longest time, and it was thought to be a disease that had a childhood onset. When diabetes occurred in adulthood it would be type 2 diabetes. But it turns out that approximately half of the cases of Type 1 diabetes may occur during adulthood right past the age of 20 or past the age of 30.
The limitations of these initial studies are that they've been in small clinics or one health system. So, it's unclear whether it's just that particular clinic or whether it applies to the general population more broadly.
We were fortunate because the CDC has collected new data that explores Type 1 diabetes in the U.S. Some of the questions they included in their national data were, “Do you have diabetes? If you do, do you have Type 1 or Type 2? And, at what age were you diagnosed?”
With these pieces of information, we were able to characterize how the age of diagnosis of Type 1 diabetes differs in the entire U.S. population.
Are Type 1 and Type 2 diabetes different diseases?
ES: They are very different diseases and have a very different burden. My whole career I have been a Type 2 diabetes epidemiologist, and I’ve been very excited to expand work with Type 1 diabetes.
There are about 1.5 million adults with Type 1 diabetes in the U.S., compared to 21 million adults with Type 2 diabetes. In terms of the total cases of diabetes, only 5 to 10 percent have Type 1 diabetes. Even in our largest epidemiologic cohorts, only a small percentage of people have Type 1 diabetes. So, we just don't have the same national data, the same epidemiologic evidence for Type 1 diabetes that we have for Type 2. The focus of our research has been trying to understand and characterize the general epidemiology and the population burden of Type 1 diabetes.
What is it about Type 1 that makes it so hard to diagnose?
MF: The presentation of symptoms varies by age of diagnosis. When it occurs in children, it tends to have a very acute presentation and the diagnosis is easier to make. When it happens in adulthood, the symptoms are often milder and it’s often misconstrued as Type 2 diabetes.
Some studies have suggested that when Type 1 diabetes occurs in adulthood, about 40% of those cases are misdiagnosed initially as Type 2 cases. Understanding how often people get diagnosed later in life is important to correctly diagnose and treat patients.
Can you talk about the different treatments?
MF: Patients with Type 1 diabetes are going to require insulin. Type 2 diabetes patients can require insulin, but that often occurs later in the disease, as oral medications become less and less effective.
ES: Because of the epidemic of overweight and obese in the general population, we’re seeing a lot of people with Type 1 diabetes who are overweight and have obesity. This can contribute to issues around misdiagnosis because people with Type 1 diabetes will have signs and will present similarly to Type 2 diabetes. They'll have insulin resistance potentially as a result of weight gain metabolic syndrome. Some people call it double diabetes—I don't like that term—but it’s this idea that if you have Type 1 diabetes, you can also have characteristics of Type 2 diabetes as well.
I understand that Type 1 used to be considered a thin person's disease, but that’s not the case anymore. MF: In a separate paper, we also explored the issue of overweight and obesity in persons with Type 1 diabetes. We found that approximately 62% of adults with Type 1 diabetes were either overweight or obese, which is comparable to the general U.S. population.
But an important disclaimer is that weight management in this population [with Type 1 diabetes] is very different. They can't just decide to go on a diet, start jogging, or engage in rigorous exercise. It can be a very, very dangerous thing to do.
Everybody's talking about Ozempic and Mounjaro—the GLP-1 drugs—for diabetes or people who are overweight to lose weight and to solve their diabetes. Where does that fit in with this population?
ES: These medications are used to treat Type 2 diabetes in the setting of obesity. Ozempic and Mounjaro are incretin hormones. They mediate satiation, reduce appetite, slow gastric emptying, and lower energy intake. They're really powerful drugs that may be helpful in Type 1 diabetes, but they're not approved for the management of obesity and Type 1 diabetes. At the moment, there aren't data to help guide their use in people with Type 1 diabetes, but I suspect they're going to be increasingly used in people with Type 1 diabetes.
MF: The other piece of managing weight—and it's thought to be foundational for Type 1 or Type 2—is dieting and exercising. However, there isn’t good guidance on how to do this in persons with Type 1 diabetes, whereas there are large and rigorous trials in Type 2 patients. We’re really just starting to figure out how to safely and effectively manage weight with lifestyle changes for Type 1 diabetics, and I think that's an important area of research that should continue moving forward.
ES: Weight management in Type 1 diabetes is complicated by insulin use and the risk of hypoglycemia, or your glucose going too low, which can be an acute complication of exercise. In people with Type 2 diabetes, we have a strong evidence base for what works. We know modest weight loss can help prevent the progression and development of Type 2 diabetes, as well as weight gain. In Type 1, we just don't have that evidence base.
Is there a concern about misdiagnosis and mistreatment? Is it possible to think a patient has Type 2 but they actually have Type 1?
MF: I think so. Insulin is the overriding concern. In the obesity paper, we looked at the percentage of people who said their doctors recommended engaging in more exercise and dieting. We found that people with Type 1 diabetes were less likely to receive the same guidance from their doctor. I think providers may be hesitant to say, “Look, just go engage in an active lifestyle.”
This is why it's important to have those studies and have that guidance so that patients and providers can be comfortable in improving lifestyle management.
Where is this research going next?
ES: What's clear from these studies is that the burden of overweight and obesity is substantial in people with Type 1 diabetes and it's not adequately managed. Going forward, I think we're going to need clinical trials, clear clinical guidelines, and patient education that addresses how best to tackle obesity in the setting of Type 1 diabetes.
It must be confusing for people with Type 1 diabetes who are hearing about people losing all this weight on these drugs, but they go to their doctor who says, “Yeah, but that's not for you.”
ES: I hope it's being handled more sensitively. These drugs are being used by all sorts of people for whom they are not indicated, and I'm sure that people with Type 1 diabetes are accessing these drugs. I think the question is, are there real safety issues? We need thoughtful discussion about this and some real evidence to make sure that we're doing more good than harm.
MF: Dr. Selvin’s group has published a paper, estimating that about 15% of people with Type 1 diabetes are on a GLP-1. But we don't have great data on what potentially can happen to individuals.
The other big part of diabetes that we hear a lot about is insulin and its price. Can you talk about your research on this topic?
MF: There was a survey that asked, “Has there been a point during the year when you were not using insulin because you couldn’t afford it?” About 20% of adults under the age of 65 said that at some point during the year, they couldn't afford their insulin and that they did engage in what sometimes is called “cost-saving rationing” [of insulin].
Medicare is now covering cheaper insulin for those over 65, but there are a lot of people for whom affordability is an issue. Can you talk more about that?
MF: The fight is not over. Just because there are national and state policies, and now manufacturers have been implementing price caps, doesn't necessarily mean that the people who need insulin the most are now able to afford it.
A recent study in the Annals of Internal Medicine looked at states that adopted or implemented out-of-pocket cost caps for insulin versus those that didn't and how that affected insulin use over time. They found that people were paying less for insulin, but the use of insulin didn't change over time. The $35 cap is an improvement, but we need to do more.
ES: There are still a lot of formulations of insulin that are very expensive. $35 a month is not cheap for someone who is on insulin for the rest of their lives.
RELATED:
- Overweight and Obesity in People With Type 1 Diabetes Nearly Same as General Population
- The Impacts of COVID-19 on Diabetes and Insulin
- Why Eli Lilly’s Insulin Price Cap Announcement Matters
Related Content

The Current and Future Outlook for Primary Health Care in South Asia

New Report Highlights U.S. 2022 Gun-Related Deaths: Firearms Remain Leading Cause of Death for Children and Teens, and Disproportionately Affect People of Color

What is Public Mental Health?

Study Estimates Home Blood Pressure Devices Don’t Fit Properly for More than 17 Million U.S. Adults
A ‘Critical Pathogen’: The Rise of Drug-Resistant Fungal Diseases
- Patient Care & Health Information
- Diseases & Conditions
- Type 1 diabetes
What is type 1 diabetes? A Mayo Clinic expert explains
Learn more about type 1 diabetes from endocrinologist Yogish Kudva, M.B.B.S.
I'm Dr. Yogish C. Kudva an endocrinologist at Mayo Clinic. In this video, we'll cover the basics of type 1 diabetes. What is it? Who gets it? The symptoms, diagnosis, and treatment. Whether you're looking for answers for yourself or someone you love. We are here to give you the best information available. Type 1 diabetes is a chronic condition that affects the insulin making cells of the pancreas. It's estimated that about 1.25 million Americans live with it. People with type 1 diabetes don't make enough insulin. An important hormone produced by the pancreas. Insulin allows your cells to store sugar or glucose and fat and produce energy. Unfortunately, there is no known cure. But treatment can prevent complications and also improve everyday life for patients with type 1 diabetes. Lots of people with type 1 diabetes live a full life. And the more we learn and develop treatment for the disorder, the better the outcome.
We don't know what exactly causes type 1 diabetes. We believe that it is an auto-immune disorder where the body mistakenly destroys insulin producing cells in the pancreas. Typically, the pancreas secretes insulin into the bloodstream. The insulin circulates, letting sugar enter your cells. This sugar or glucose, is the main source of energy for cells in the brain, muscle cells, and other tissues. However, once most insulin producing cells are destroyed, the pancreas can't produce enough insulin, meaning the glucose can't enter the cells, resulting in an excess of blood sugar floating in the bloodstream. This can cause life-threatening complications. And this condition is called diabetic ketoacidosis. Although we don't know what causes it, we do know certain factors can contribute to the onset of type 1 diabetes. Family history. Anyone with a parent or sibling with type 1 diabetes has a slightly increased risk of developing it. Genetics. The presence of certain genes can also indicate an increased risk. Geography. Type 1 diabetes becomes more common as you travel away from the equator. Age, although it can occur at any age there are two noticeable peaks. The first occurs in children between four and seven years of age and the second is between 10 and 14 years old.
Signs and symptoms of type 1 diabetes can appear rather suddenly, especially in children. They may include increased thirst, frequent urination, bed wetting in children who previously didn't wet the bed. Extreme hunger, unintended weight loss, fatigue and weakness, blurred vision, irritability, and other mood changes. If you or your child are experiencing any of these symptoms, you should talk to your doctor.
The best way to determine if you have type 1 diabetes is a blood test. There are different methods such as an A1C test, a random blood sugar test, or a fasting blood sugar test. They are all effective and your doctor can help determine what's appropriate for you. If you are diagnosed with diabetes, your doctor may order additional tests to check for antibodies that are common in type 1 diabetes in the test called C-peptide, which measures the amount of insulin produced when checked simultaneously with a fasting glucose. These tests can help distinguish between type 1 and type 2 diabetes when a diagnosis is uncertain.
If you have been diagnosed with type 1 diabetes, you may be wondering what treatment looks like. It could mean taking insulin, counting carbohydrates, fat protein, and monitoring your glucose frequently, eating healthy foods, and exercising regularly to maintain a healthy weight. Generally, those with type 1 diabetes will need lifelong insulin therapy. There are many different types of insulin and more are being developed that are more efficient. And what you may take may change. Again, your doctor will help you navigate what's right for you. A significant advance in treatment from the last several years has been the development and availability of continuous glucose monitoring and insulin pumps that automatically adjust insulin working with the continuous glucose monitor. This type of treatment is the best treatment at this time for type 1 diabetes. This is an exciting time for patients and for physicians that are keen to develop, prescribe such therapies. Surgery is another option. A successful pancreas transplant can erase the need for additional insulin. However, transplants aren't always available, not successful and the procedure can pose serious risks. Sometimes it may outweigh the dangers of diabetes itself. So transplants are often reserved for those with very difficult to manage conditions. A successful transplant can bring life transforming results. However, surgery is always a serious endeavor and requires ample research and concentration from you, your family, and your medical team.
The fact that we don't know what causes type 1 diabetes can be alarming. The fact that we don't have a cure for it even more so. But with the right doctor, medical team and treatment, type 1 diabetes can be managed. So those who live with it can get on living. If you would like to learn even more about type 1 diabetes, watch our other related videos or visit mayoclinic.org. We wish you well.
Type 1 diabetes, once known as juvenile diabetes or insulin-dependent diabetes, is a chronic condition. In this condition, the pancreas makes little or no insulin. Insulin is a hormone the body uses to allow sugar (glucose) to enter cells to produce energy.
Different factors, such as genetics and some viruses, may cause type 1 diabetes. Although type 1 diabetes usually appears during childhood or adolescence, it can develop in adults.
Even after a lot of research, type 1 diabetes has no cure. Treatment is directed toward managing the amount of sugar in the blood using insulin, diet and lifestyle to prevent complications.
Products & Services
- A Book: The Essential Diabetes Book
Type 1 diabetes symptoms can appear suddenly and may include:
- Feeling more thirsty than usual
- Urinating a lot
- Bed-wetting in children who have never wet the bed during the night
- Feeling very hungry
- Losing weight without trying
- Feeling irritable or having other mood changes
- Feeling tired and weak
- Having blurry vision
When to see a doctor
Talk to your health care provider if you notice any of the above symptoms in you or your child.
The exact cause of type 1 diabetes is unknown. Usually, the body's own immune system — which normally fights harmful bacteria and viruses — destroys the insulin-producing (islet) cells in the pancreas. Other possible causes include:
- Exposure to viruses and other environmental factors
The role of insulin
Once a large number of islet cells are destroyed, the body will produce little or no insulin. Insulin is a hormone that comes from a gland behind and below the stomach (pancreas).
- The pancreas puts insulin into the bloodstream.
- Insulin travels through the body, allowing sugar to enter the cells.
- Insulin lowers the amount of sugar in the bloodstream.
- As the blood sugar level drops, the pancreas puts less insulin into the bloodstream.
The role of glucose
Glucose — a sugar — is a main source of energy for the cells that make up muscles and other tissues.
- Glucose comes from two major sources: food and the liver.
- Sugar is absorbed into the bloodstream, where it enters cells with the help of insulin.
- The liver stores glucose in the form of glycogen.
- When glucose levels are low, such as when you haven't eaten in a while, the liver breaks down the stored glycogen into glucose. This keeps glucose levels within a typical range.
In type 1 diabetes, there's no insulin to let glucose into the cells. Because of this, sugar builds up in the bloodstream. This can cause life-threatening complications.
Risk factors
Some factors that can raise your risk for type 1 diabetes include:
- Family history. Anyone with a parent or sibling with type 1 diabetes has a slightly higher risk of developing the condition.
- Genetics. Having certain genes increases the risk of developing type 1 diabetes.
- Geography. The number of people who have type 1 diabetes tends to be higher as you travel away from the equator.
- Age. Type 1 diabetes can appear at any age, but it appears at two noticeable peaks. The first peak occurs in children between 4 and 7 years old. The second is in children between 10 and 14 years old.
Complications
Over time, type 1 diabetes complications can affect major organs in the body. These organs include the heart, blood vessels, nerves, eyes and kidneys. Having a normal blood sugar level can lower the risk of many complications.
Diabetes complications can lead to disabilities or even threaten your life.
- Heart and blood vessel disease. Diabetes increases the risk of some problems with the heart and blood vessels. These include coronary artery disease with chest pain (angina), heart attack, stroke, narrowing of the arteries (atherosclerosis) and high blood pressure.
Nerve damage (neuropathy). Too much sugar in the blood can injure the walls of the tiny blood vessels (capillaries) that feed the nerves. This is especially true in the legs. This can cause tingling, numbness, burning or pain. This usually begins at the tips of the toes or fingers and spreads upward. Poorly controlled blood sugar could cause you to lose all sense of feeling in the affected limbs over time.
Damage to the nerves that affect the digestive system can cause problems with nausea, vomiting, diarrhea or constipation. For men, erectile dysfunction may be an issue.
- Kidney damage (nephropathy). The kidneys have millions of tiny blood vessels that keep waste from entering the blood. Diabetes can damage this system. Severe damage can lead to kidney failure or end-stage kidney disease that can't be reversed. End-stage kidney disease needs to be treated with mechanical filtering of the kidneys (dialysis) or a kidney transplant.
- Eye damage. Diabetes can damage the blood vessels in the retina (part of the eye that senses light) (diabetic retinopathy). This could cause blindness. Diabetes also increases the risk of other serious vision conditions, such as cataracts and glaucoma.
- Foot damage. Nerve damage in the feet or poor blood flow to the feet increases the risk of some foot complications. Left untreated, cuts and blisters can become serious infections. These infections may need to be treated with toe, foot or leg removal (amputation).
- Skin and mouth conditions. Diabetes may leave you more prone to infections of the skin and mouth. These include bacterial and fungal infections. Gum disease and dry mouth also are more likely.
- Pregnancy complications. High blood sugar levels can be dangerous for both the parent and the baby. The risk of miscarriage, stillbirth and birth defects increases when diabetes isn't well-controlled. For the parent, diabetes increases the risk of diabetic ketoacidosis, diabetic eye problems (retinopathy), pregnancy-induced high blood pressure and preeclampsia.
There's no known way to prevent type 1 diabetes. But researchers are working on preventing the disease or further damage of the islet cells in people who are newly diagnosed.
Ask your provider if you might be eligible for one of these clinical trials. It is important to carefully weigh the risks and benefits of any treatment available in a trial.
- Summary of revisions: Standards of medical care in diabetes — 2022. Diabetes Care. 2022; doi:10.2337/dc22-Srev.
- Papadakis MA, et al., eds. Diabetes mellitus. In: Current Medical Diagnosis & Treatment 2022. 61st ed. McGraw Hill; 2022. https://accessmedicine.mhmedical.com. Accessed May 4, 2022.
- What is diabetes? National Institute of Diabetes and Digestive and Kidney Diseases. https://www.niddk.nih.gov/health-information/diabetes/overview/what-is-diabetes. Accessed May 4, 2022.
- Levitsky LL, et al. Epidemiology, presentation, and diagnosis of type 1 diabetes mellitus in children and adolescents. https://www.uptodate.com/contents/search. Accessed May 4, 2022.
- Diabetes mellitus (DM). Merck Manual Professional Version. https://www.merckmanuals.com/professional/endocrine-and-metabolic-disorders/diabetes-mellitus-and-disorders-of-carbohydrate-metabolism/diabetes-mellitus-dm. Accessed May 4, 2022.
- AskMayoExpert. Type 1 diabetes mellitus. Mayo Clinic; 2021.
- Robertson RP. Pancreas and islet transplantation in diabetes mellitus. https://www.uptodate.com/contents/search. Accessed May 4, 2022.
- Levitsky LL, et al. Management of type 1 diabetes mellitus in children during illness, procedures, school, or travel. https://www.uptodate.com/contents/search. Accessed May 4, 2022.
- Hyperglycemia (high blood glucose). American Diabetes Association. https://www.diabetes.org/healthy-living/medication-treatments/blood-glucose-testing-and-control/hyperglycemia. Accessed May 4, 2022.
- Diabetes and DKA (ketoacidosis). American Diabetes Association. https://www.diabetes.org/diabetes/dka-ketoacidosis-ketones. Accessed May 4, 2022.
- Insulin resistance & prediabetes. National Institute of Diabetes and Digestive and Kidney Diseases. https://www.niddk.nih.gov/health-information/diabetes/overview/what-is-diabetes/prediabetes-insulin-resistance. Accessed May 4, 2022.
- Blood sugar and insulin at work. American Diabetes Association. https://www.diabetes.org/tools-support/diabetes-prevention/high-blood-sugar. Accessed May 4, 2022.
- Inzucchi SE, et al. Glycemic control and vascular complications in type 1 diabetes. https://www.uptodate.com/contents/search. Accessed May 4, 2022.
- Diabetes and oral health. American Diabetes Association. https://www.diabetes.org/diabetes/keeping-your-mouth-healthy. Accessed May 4, 2022.
- Drug treatment of diabetes mellitus. Merck Manual Professional Version. https://www.merckmanuals.com/professional/endocrine-and-metabolic-disorders/diabetes-mellitus-and-disorders-of-carbohydrate-metabolism/drug-treatment-of-diabetes-mellitus. Accessed May 4, 2022.
- Weinstock DK, et al. Management of blood glucose in adults with type 1 diabetes mellitus. https://www.uptodate.com/contents/search. Accessed May 7, 2022.
- FDA proves first automated insulin delivery device for type 1 diabetes. U.S. Food and Drug Administration. https://www.fda.gov/news-events/press-announcements/fda-approves-first-automated-insulin-delivery-device-type-1-diabetes. Accessed May 4, 2022.
- Boughton CK, et al. Advances in artificial pancreas systems. Science Translational Medicine. 2019; doi:10.1126/scitranslmed.aaw4949.
- Hypoglycemia (low blood sugar). American Diabetes Association. https://www.diabetes.org/healthy-living/medication-treatments/blood-glucose-testing-and-control/hypoglycemia. Accessed May 4, 2022.
- Diabetes in the workplace and the ADA. U.S. Equal Opportunity Employment Commission. https://www.eeoc.gov/laws/guidance/diabetes-workplace-and-ada. Accessed May 4, 2022.
- Cardiovascular disease and risk management: Standards of medical care in diabetes — 2022. Diabetes Care. 2022; doi:10.2337/dc22-S010.
- Diabetes technology. Standards of Medical Care in Diabetes — 2022. 2022; doi:10.2337/dc22-S007.
- FDA authorizes a second artificial pancreas system. JDRF. https://www.jdrf.org/blog/2019/12/13/jdrf-reports-fda-authorizes-second-artificial-pancreas-system/. Accessed May 4, 2022.
- Classification and diagnosis of diabetes: Standards of medical care in diabetes — 2022. Diabetes Care. 2022; doi:10.2337/dc22-S002.
- Retinopathy, neuropathy, and foot care: Standards of medical care in diabetes — 2022. Diabetes Care. 2022; doi:10.2337/dc22-S012.
- Glycemic targets: Standards of medical care in diabetes — 2022. Diabetes Care. 2022; doi:10.2337/dc22-S012.
- Pharmacologic approaches to glycemic treatment: Standards of medical care in diabetes — 2022. Diabetes Care. 2022; doi:10.2337/dc22-S009.
- Facilitating behavior change and well-being to improve health outcomes: Standards of medical care in diabetes — 2022. Diabetes Care. 2022; doi:10.2337/dc22-S005.
- Centers for Disease Control and Prevention. Use of hepatitis B vaccination for adults with diabetes mellitus: Recommendations of the Advisory Committee on Immunization Practices (ACIP). Morbidity and Mortality Weekly Report. 2011;60:1709.
- Management of diabetes in pregnancy: Standards of medical care in diabetes — 2022. Diabetes Care. 2022; doi:10.2337/dc22-S015.
- Older adults: Standards of medical care in diabetes — 2022. Diabetes Care. 2022; doi:10.2337/dc22-S013.
- FDA approves first-of-its-kind automated insulin delivery and monitoring system for use in young pediatric patients. U.S. Food and Drug Administration. https://www.fda.gov/news-events/press-announcements/fda-approves-first-its-kind-automated-insulin-delivery-and-monitoring-system-use-young-pediatric#:~:text=Today, the U.S. Food and,by individuals aged 2 to. Accessed May 8, 2022.
- What you need to know: Getting a COVID-19 vaccine. American Diabetes Association. https://www.diabetes.org/coronavirus-covid-19/vaccination-guide. Accessed June 1, 2022.
News from Mayo Clinic
- Driven by family, fueled by hope: Mayo Clinic researcher fights against Type 1 diabetes Aug. 06, 2023, 11:00 a.m. CDT
- Symptoms & causes
- Diagnosis & treatment
- Doctors & departments
Mayo Clinic does not endorse companies or products. Advertising revenue supports our not-for-profit mission.
- Opportunities
Mayo Clinic Press
Check out these best-sellers and special offers on books and newsletters from Mayo Clinic Press .
- Mayo Clinic on Incontinence - Mayo Clinic Press Mayo Clinic on Incontinence
- The Essential Diabetes Book - Mayo Clinic Press The Essential Diabetes Book
- Mayo Clinic on Hearing and Balance - Mayo Clinic Press Mayo Clinic on Hearing and Balance
- FREE Mayo Clinic Diet Assessment - Mayo Clinic Press FREE Mayo Clinic Diet Assessment
- Mayo Clinic Health Letter - FREE book - Mayo Clinic Press Mayo Clinic Health Letter - FREE book
5X Challenge
Thanks to generous benefactors, your gift today can have 5X the impact to advance AI innovation at Mayo Clinic.
Warning: The NCBI web site requires JavaScript to function. more...
An official website of the United States government
The .gov means it's official. Federal government websites often end in .gov or .mil. Before sharing sensitive information, make sure you're on a federal government site.
The site is secure. The https:// ensures that you are connecting to the official website and that any information you provide is encrypted and transmitted securely.
- Publications
- Account settings
- Browse Titles
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-.

StatPearls [Internet].
Type 1 diabetes.
Jessica Lucier ; Scott C. Dulebohn .
Last Update: March 3, 2023 .
- Continuing Education Activity
Type 1 diabetes mellitus (T1D) is an autoimmune disease that leads to the destruction of insulin-producing pancreatic beta cells. Individuals with T1D require life-long insulin replacement with multiple daily insulin injections daily, insulin pump therapy, or the use of an automated insulin delivery system. Without insulin, diabetic ketoacidosis (DKA) develops and is life-threatening. In addition to insulin therapy, glucose monitoring with (preferably) a continuous glucose monitor (CGM) and a blood glucose monitor if CGM is unavailable is recommended. Self-management education and support should include training on monitoring, insulin administration, ketone testing when indicated, nutrition including carbohydrate estimates, physical activity, ways of avoiding and treating hypoglycemia, and use of sick day rules. Psychosocial issues also need to be recognized and addressed. This activity reviews the evaluation and management of T1D. It highlights the importance of a multidisciplinary approach to enhance outcomes.
- Describe the pathophysiology of type 1 diabetes mellitus.
- Explain the management of type 1 diabetes mellitus.
- Review other conditions for which patients with type 1 diabetes mellitus are at increased risk of developing.
- Explain the importance of improving coordination amongst the interprofessional team to enhance care for patients affected by type 1 diabetes mellitus.
- Introduction
Type 1 diabetes mellitus (T1D) is an autoimmune disease that leads to the destruction of insulin-producing pancreatic beta cells. There is heterogeneity in the metabolic, genetic, and immunogenetic characteristics of T1D and age-related differences, requiring a personalized approach for each individual. Loss of insulin secretion can occur quickly or gradually. Residual insulin production (detectable/higher c-peptide) is more common in adult-onset compared to youth-onset T1D, whereas diabetic ketoacidosis is more common in youth with T1D. [1] Detectable c-peptide is associated with better glycemic control. [2] The presence of other autoimmune conditions, obesity, comorbidities, and the development of diabetes-related complications is also variable. [3]
Successful management of T1D requires multiple daily insulin injections (MDI), insulin pump therapy, or the use of an automated insulin delivery system, as well as glucose monitoring, preferably with a continuous glucose monitor (CGM). All people with T1D should be able to perform capillary blood glucose monitoring (BGM) if CGM is unavailable. Self-management education, training, and support, as well as addressing psychosocial issues, help to optimize outcomes. A collaborative multidisciplinary approach, utilizing medical providers, nurse and dietitian educators, pharmacists, community resources, and specialists as needed (including podiatrists, mental health professionals, social workers, ophthalmologists, cardiologists, and others), is recommended. [4]
In T1D, there is autoimmune destruction of the beta cells in the pancreatic islets over months or years, causing an absolute deficiency of insulin. Although the exact etiology of T1D is still unknown, researchers believe there is a genetic predisposition with a strong link with specific HLA (DR and DQ) alleles. This association is more pronounced in youth-onset T1D compared to adult-onset T1D. [5] Multiple other genes contribute to heritability as well. [6]
In those at risk, it is generally believed that viruses, environmental including dietary factors, and/or other stressors can trigger autoimmune beta-cell destruction. Some studies have found an increased risk of development of T1D related to infection with Coxsackie virus, enteroviruses, cytomegalovirus, rubella virus, influenza B, mumps virus, and more recently, SARS-CoV-2 (COVID-19). [7] [8] [9] In The Environmental Determinants of Diabetes in the Young (TEDDY) study, breastfeeding was not associated with the risk of islet autoimmunity in children genetically at increased risk. However, a systematic review and meta-analysis concluded that breastfeeding and the later introduction of gluten, fruit, and cow’s milk were associated with a lower risk of developing T1D. [10] Research to better understand the etiology of T1D is ongoing.
The presence of circulating pancreatic islet autoantibodies suggests that the individual is at risk for or has developed T1D. These antibodies include islet cell cytoplasmic antibodies (ICA), antibodies to insulin (IAA), glutamic acid decarboxylase isoform 65 (GAD65), insulinoma antigen 2/islet tyrosine phosphatase 2 (IA-2) and zinc transporter isoform 8 (ZnT8). IAAs are primarily detected in children. [11] GAD65 is the most common autoantibody detected in adults [3] . ICA is no longer routinely recommended, as it is an imprecise assay. The greater the number of detectable antibodies and the higher their titers, the greater the risk of developing T1D.
- Epidemiology
T1D is one of the most frequent chronic diseases in children but can have its onset at any age. In adults, new-onset type 1 diabetes may be misdiagnosed as type 2 diabetes and is more common than youth-onset T1D. [3] [ [5] There has been a steady increase in the incidence and prevalence of T1D, representing approximately 5% to 10% of people with diabetes. A systematic review and meta-analysis reported that the worldwide prevalence of T1D was 9.5%, with an incidence of 15 per 100,000 people. [12] Worldwide, there is also a considerable geographic variation in incidence. The highest reported incidences are in Finland and other Northern European nations, with rates approximately 400 times greater than those seen in China and Venezuela, where there is the lowest reported incidence.
- Pathophysiology
The development of T1D occurs in 3 stages. Stage 1 is asymptomatic and characterized by normal fasting glucose, normal glucose tolerance, and the presence of ≥2 pancreatic autoantibodies. Stage 2 diagnostic criteria include the presence of pancreatic autoantibodies (usually multiple) and dysglycemia: impaired fasting glucose (fasting glucose 100 to 125 mg/dL) or impaired glucose tolerance (2-hour post-75 gm glucose load glucose 140 to 199 mg/dL) or an HbA1c 5.7% to 6.4%. Individuals remain asymptomatic. In stage 3, there is diabetes, defined by hyperglycemia (random glucose ≥200 mg/dL) with clinical symptoms, fasting glucose ≥126 mg/dL, glucose ≥200 mg/dL two hours after ingesting 75 g of glucose during an oral glucose tolerance test and/or HbA1c ≥6.5%. If the individual lacks classic symptoms of hyperglycemia or hyperglycemic crisis, it is recommended that two tests be performed (simultaneously or at different times) to confirm the diagnosis. If there is an acute onset of symptoms with hyperglycemia, as more often occurs in youth-onset T1D, HbA1c may be misleading at the time of diagnosis, and glucose criteria should be used. [4]
T1D, especially in children, classically presents with hyperglycemic symptoms, which can be sudden, and include polydipsia, polyuria, polyphagia, nocturnal enuresis, blurred vision, unintentional weight loss, fatigue, and weakness. If not evaluated and treated promptly, it can become a medical emergency. In addition to hyperglycemia, electrolyte abnormalities may be present. If these individuals are not treated, DKA can develop, requiring hospitalization and treatment with intravenous fluids, insulin, potassium, and careful monitoring. Almost one-third of youth present with DKA. [13]
In adult-onset diabetes, the onset of symptoms is more variable than in youth, and DKA is less common. It can be difficult to distinguish T1D and type 2 diabetes. GAD65 should be the initial antibody tested when diagnosing T1D in adults is suspected. If negative and/or if available, IA2 and/or ZNT8 should be measured as well. C-peptide levels can be used when there is a question about which type of diabetes is present. A random C-peptide should be drawn with concurrent serum glucose. If the duration of diabetes exceeds three years, c-peptide >600 pmol/L strongly suggests type 2 diabetes. A low (<200 pmol/L) or undetectable c-peptide confirms the diagnosis of T1D. [3]
- History and Physical
At the initial outpatient visit, obtaining a complete medical, surgical, psychosocial, and family history, including pregnancy and contraception history, is essential. History of prior diabetes education, monitoring of BG and ketones, use of CGM, administration of insulin, recognition/treatment of hypoglycemia, use of glucagon, diet, physical activity, smoking and alcohol use, understanding of sick-day rules, ability to problem solve and immunization history, should also be obtained. Particular attention should be paid to the date of diagnosis, prior treatment, current medications, presence of hypoglycemia unawareness, and history of acute complications (hypoglycemia including severe episodes and episodes of DKA) and chronic complications (skin disorders, dental problems, retinopathy, macular edema, neuropathy, kidney disease, cardiovascular disease, peripheral arterial disease, stroke, foot ulcers, amputations, hearing loss, sleep disorders). Since people with type 1 diabetes are at increased risk of other autoimmune disorders, including autoimmune thyroid disease and celiac disease, the history should also focus on these conditions. [3]
Clinicians should measure height, weight, and blood pressure. The skin should be examined, especially at insulin injection or infusion sites. If lipodystrophy is evident, they should be educated on the importance of varying insulin injection/infusion sites. The thyroid, heart, chest, and abdomen should also be examined. A foot exam is performed to examine pedal pulses and detect foot deformities, pre-ulcerative lesions, ulcerations, calluses, and onychomycosis. It is also important to test vibratory and protective sensations; abnormal testing with a 10-g monofilament exam suggests an increased risk of ulceration.
When screening for psychosocial issues, a number of measures are available such as the Patient Health Questionnaire (PHQ-2/PHQ-9) for Depression and Generalized Anxiety Disorder (GAD-7). Diabetes distress and social determinants of health should be assessed. Since eating disorders are more common in type 1 diabetes, particularly in young women, evaluation should be considered clinically indicated. Early cognitive decline is also common, so cognitive testing should be considered when impairment is suspected. [3]
Data from CGMs, blood glucose meters, insulin pumps, and automated insulin delivery systems should be downloaded, examined, and discussed at each visit and between visits when needed to adjust treatment regimens to achieve glycemic goals.
CGMs are devices that measure glucose in interstitial fluid and are extremely useful tools for people with T1D. Sensors are inserted into the subcutaneous tissue and transmit glucose readings every 5 minutes to a receiver where they can be displayed in real-time. One can examine trends and use low and high glucose alarms to prevent serious hypoglycemia and hyperglycemia episodes. Alarms can also alert to a rapid change in glucose value. Readings from certain CGM sensors can be transmitted to smartphones and can be shared with relatives, friends, or caregivers. A less expensive CGM option uses a “reader” (a device the user scans over the site of sensor placement) or a smartphone to visualize recent glucose readings and trends. All these devices make it easier to monitor glucose values throughout the day and night. Users examine trends and are provided with important information to guide insulin therapy and food intake to help avoid wide glycemic excursions and hypoglycemia.
Data from CGMs can be uploaded and stored in cloud-based systems. These data include percent: Time in range TIR, usually 70 to 180 mg/dL; TIR targets are lower during pregnancy and higher in those who are frail and/or with complex comorbidities or limited life expectancy), time below range (TBR; <70 mg/dL; level 1 hypoglycemia is 54-69 mg/dL and level 2 hypoglycemia is <54 mg/dL); time above range (TAR; usually >180 mg/dL; level 1 hyperglycemia is 181 to 250 mg/dL and level 2 hyperglycemia is >250 mg/dL); and glycemic variability (% CV; coefficient of variation). These data should be reviewed with the goal of understanding factors contributing to hypoglycemia and hyperglycemia and to help guide insulin dosing, diet, and physical activity to achieve goals. A primary goal should be minimizing hypoglycemia. A higher percent TIR is associated with decreased diabetes-related complications. [14] [15] HbA1c, TIR, and TBR improve when MDI or pump therapy is augmented with CGM use. The glucose management indicator (GMI) is calculated using average sensor readings over a 14-day period and correlates with the estimated HbA1c. [16]
When CGM data are unavailable, examination of BG data fasting, pre-meal, 1 to 3 hours postprandial (when adjusting prandial dosing), bedtime, when hypoglycemia is suspected, and occasionally in the middle of the night, should be used to direct insulin dosing. Insulin dosing data from connected insulin pens and pumps should also be discussed.
HbA1c is recommended every 3 to 6 months. The HbA1c reflects glycemic control over the previous 2 to 3 months. A typical goal HbA1c is <7.0%, with higher goals in people with frailty, cardiovascular disease/multiple comorbidities, history of severe hypoglycemia, and/or hypoglycemia unawareness. Lower goals are used when they can be achieved safely (without an increase in hypoglycemia).
Other laboratory tests include a yearly lipid profile, serum creatinine, eGFR, and urine albumin to creatinine ratio. Serum potassium should be monitored if taking an ACE-I, ARB, or diuretic, and AST, ALT, TSH, celiac screen, vitamin B12, and vitamin D at least once and as indicated clinically. These tests could be repeated more frequently if the previous results were abnormal. Since people with T1D are at an increased risk of developing other autoimmune diseases, such as autoimmune thyroid disease, celiac disease, primary adrenal insufficiency, and rheumatoid arthritis, screening for autoimmune disorders should be considered when clinically appropriate. [17] [4]
- Treatment / Management
People with T1D require insulin therapy, glucose monitoring (preferably CGM), and diabetes self-management education and support. Multiple daily insulin injections (MDI) using basal (preferably a long-acting insulin) and bolus (preferably rapid-acting insulin for meals and correction)insulins, continuous subcutaneous insulin infusion (rapid-acting insulin) through an insulin pump, or use of automated insulin delivery (hybrid closed loop) systems with rapid-acting insulin, are available. Automated insulin delivery is associated with greater time in the target range and less hypoglycemia. When initiating a treatment plan, use shared decision-making, considering individualized realistic and attainable goals, risk of hypoglycemia, lifestyle, and the availability and affordability of different regimens. [4]
Hypoglycemia is the most frequent adverse effect of insulin therapy. It is important to educate people with diabetes and their partners about the signs and symptoms of hypoglycemia, which include diaphoresis, tachycardia, lightheadedness, confusion, hunger, visual changes, and tremors. With a long duration of T1D, hypoglycemia unawareness becomes more common. Generally, 15 to 20 g of glucose should be given orally for blood glucose below 70 mg/dL. [17] Glucose readings should be rechecked 15 minutes later, with additional carbohydrates given if needed.d Once the glucose reading has normalized, if glucose readings again begin to fall, a snack should be given to prevent a recurrence. Glucagon should be prescribed for emergency use for severe hypoglycemia (when there is an inability to consume carbohydrates by mouth). People with T1D should also receive sick day instructions, including how to manage hyperglycemia and ketone testing. When initiating insulin therapy in an adult, the person’s weight in kilograms is multiplied by 0.2 to 0.6 units to calculate the initial total daily insulin dose (TDD). Generally, basal requirements are 40% to 50% of the TDD, and the rest approximates the daily rapid-acting insulin that must be given before or with meals. Dosing is modified based on many factors, including diet, physical activity, and CGM and/or BGM results.
When possible, people with T1D should meet with a dietitian, be taught carbohydrate counting, and be instructed to use an insulin-to-carbohydrate ratio (grams of carbohydrate covered by one unit of insulin) for mealtime dosing. If carbohydrate counting is not possible, a carbohydrate-consistent diet is helpful. Estimating the fall in glucose resulting from 1 unit of rapid-acting insulin, called a correction or insulin sensitivity factor, is also recommended when treating hyperglycemia. The correction factor can be initially estimated using the formula 1800 divided by the TDD. This number will need to be adjusted per subsequent glucose monitoring results. When using correction doses, the individual needs to be careful not to take injections too close together (“stacking”) to avoid overdosing (insulin administered when there is still active insulin from previous doses causing overlapping insulin doses) and hypoglycemia.
It is important to note that insulin requirements vary across the lifespan and under specific circumstances. For example, larger insulin doses are typically required during puberty, pregnancy, when steroids are given, and with the development of obesity. Individuals need less insulin when they are engaged in aerobic exercise and during the “honeymoon period.” The honeymoon period occurs soon after diagnosis when there can be a temporary recovery of beta-cell function.
Multiple types of insulin can be used for insulin injection therapy. [18] Rapid-acting insulin (lispro, aspart, glulisine) will generally have onset in 12 to 30 minutes, peak in 1 to 3 hours, and have a duration of action of 3-6 hours. Ultra-rapid-acting lispro or aspart have a slightly quicker onset of action and somewhat shorter duration of action. . Short-acting insulin (regular insulin) has an onset in 30 minutes to 1 hour and peak in 2 to 4 hours with a duration of 5 to 8 hours.
For basal insulin injection therapy, long-acting insulin is preferred, often given once a day (U-100 and U-300 glargine, degludec) or 1 to 2 times daily (detemir and U-100 glargine). Glargine does not have a pronounced peak and lasts approximately 20 to 24 hours. U-300 glargine lasts more than 24 hours, and degludec has a longer duration of action, up to 42 hours. Intermediate insulin (NPH, NPL) is the least expensive basal insulin, but it is associated with more hypoglycemia. It has onset in 1 to 2 hours, peak action at 2 to 8 hours, duration of 12 to 24 hours, and is usually given before breakfast and bedtime. When MDI is used, the individual will ideally use rapid-acting insulin with each meal for hyperglycemia correction and a daily long-acting basal insulin.
Insulin pumps deliver insulin every 5 minutes to provide basal needs and deliver boluses of insulin to control mealtime excursions and correct hyperglycemia. Only rapid-acting insulin is used in insulin pumps/automated insulin delivery systems. Some pumps use external tubing to infuse insulin from the pump to the infusion site in the subcutaneous tissue, while another pump uses a “pod” that contains insulin, which is directly applied to the skin and is controlled via a wireless connection to a controller or smartphone. Insulin pumps are programmed with adjustable basal rates, insulin-to-carbohydrate ratios, correction factors, and target glucose ranges.
Some insulin pumps communicate with CGMs and have threshold/predictive low-glucose suspend features. With these devices, insulin delivery is suspended when hypoglycemia occurs or is predicted to occur. In the newer hybrid closed-loop automated insulin delivery systems, the CGM sends glucose data to an insulin pump with a control algorithm. Basal insulin delivery is automated based on the CGM readings received every 5 minutes and the target glucose. Advanced systems deliver automated correction boluses as well. Mealtime bolus insulin is still required to be delivered under the direction of the user.
Several clinical trials are currently underway, testing “closed-loop” fully automated insulin delivery systems, as well as a closed-loop system that delivers insulin and glucagon. The hope is that these closed-loop automated insulin systems will lead to better glucose management, with minimal risk of hypoglycemia and reduced burden for people with T1D.
Physical activity is recommended for people with T1D. Exercise increases insulin sensitivity, improves cardiovascular health, improves lipid profiles, decreases microvascular complications, reduces the risk of osteoporosis, and decreases mortality. Glycemic control can be more difficult during times of activity related to the intensity and duration of the activity, amount of circulating insulin, glucose level before exercise, and dietary intake. Individuals should be taught the effect of different types of activity (aerobic vs. anaerobic) on glucose levels, how to balance carbohydrate intake and insulin doses when active, and how to avoid hypoglycemia and wide glycemic excursions with exercise.
In addition to insulin therapy, diet, and physical activity, individuals with T1D should generally have an annual eye exam by an eye care specialist and an annual foot exam. Those with foot deformities, neuropathy, a history of foot ulcers, or peripheral arterial disease should have their feet examined at each visit, be educated in proper foot care/footwear, and, if available, see a podiatrist and be evaluated for orthotics if indicated. Other specialists, such as nephrologists, ophthalmologists, and cardiologists, as well as referrals to community resources, social workers, and mental health professionals, may be needed. The use of statins and other anti-hyperlipidemic therapy, smoking cessation, and anti-hypertension therapy to reduce cardiovascular risk and risk of nephropathy and retinopathy are important and discussed later in this article. Pancreatic and islet cell transplantation are two treatment options that can restore normoglycemia.
A pancreatic transplant is usually performed simultaneously with a kidney transplant (SPK transplant). These transplants are considered when end-stage renal disease is present, in relatively younger individuals (<50 years old without coronary artery disease), and when usual treatment options have been unsuccessful in preventing large variability and severe hypoglycemia. Individuals who receive a pancreatic transplant or an islet-cell transplantation require immunosuppressive therapy. Encapsulated islets could obviate the need for immunosuppressive therapy and are a promising future therapy. These and other research initiatives give hope to the increasing number of people with T1D that a cure is in their future. [4]
- Differential Diagnosis
- Diabetes mellitus type 2
- Pancreatic diabetes
- Steroid-induced diabetes
- Diabetes insipidus
- Factitious illness
- Psychogenic polydipsia
- Renal glycosuria
With better glucose, blood pressure, lipid control, and better foot care, there has been a reduction in the morbidity and mortality associated with T1D. Rates of serious diabetes-related complications are lower; if present, their onset has been delayed for many. Although people with T1D have 2 to 5-fold higher mortality than those without diabetes, mortality rates have declined. This is discussed further in other sections. [19]
- Complications
The major acute complications of diabetes are hypoglycemia and serious hyperglycemia, including diabetic ketoacidosis. The major chronic complications are listed below:
- Nephropathy
- Neuropathy: peripheral and autonomic
- Retinopathy/macular edema
- Heart disease, including coronary artery disease, heart failure, cardiomyopathy
- Peripheral arterial disease
- Cerebrovascular disease, including stroke and TIA
- Hearing loss
- Diabetic foot diseases, including foot ulcers and amputations
- Deterrence and Patient Education
Patient medication compliance and follow-up with specialists and educators are critical factors in preventing complications. At every patient encounter, the pharmacist, nurse, and clinicians should emphasize the importance of blood glucose control, long-term complications, and management goals. The patient should be encouraged to modify their lifestyle to reduce the risk of complications. In addition, all patients with diabetes should be made aware of the signs and symptoms of hypoglycemia and ways of managing it. Patients should be educated about available resources and the benefits of joining support groups. A dietitian should educate the patient about foods that can be consumed, and the nurse should educate the patient on blood glucose monitoring at home.
- Enhancing Healthcare Team Outcomes
Self-management of T1D includes administering insulin multiple times daily with glucose monitoring and attention to food intake and physical activity every day, which is a considerable burden. Whereas newer technologies have helped people improve their glycemic control, they are costly, complex, and require education and training. Many people with diabetes fear hypoglycemia, hyperglycemia, and the development of complications, and depression, anxiety, and eating disorders can develop. The medical, education, training, psychological, and social challenges faced by people with T1D daily are best addressed by an interprofessional team that includes clinicians (MDs, DOs, NPs, and PAs), nurses (including diabetes nurse educators), pharmacists, dieticians, mental health professionals, social workers, podiatrists, and the use of community resources. Individualized treatment approaches, which can reduce the burden and further improve outcomes, are needed, and the interprofessional care model will yield the best possible patient outcomes. [3]
It is imperative for all interprofessional team members to coordinate their activities and interventions with the rest of the team and utilize open communication channels to ensure everyone involved in patient care, as well as the patient themselves, has access to the same accurate, updated patient information. Nurses are often crucial in coordinating activities between various professionals on the case and play a role in patient evaluation, education, and monitoring. Pharmacists should work directly with diabetes educators to ensure proper insulin dosing and participate in patient medication education and reconciliation. These examples of interprofessional care will help drive improved patient outcomes. [Level 5]
- Review Questions
- Access free multiple choice questions on this topic.
- Comment on this article.
Disclosure: Jessica Lucier declares no relevant financial relationships with ineligible companies.
Disclosure: Scott Dulebohn declares no relevant financial relationships with ineligible companies.
This book is distributed under the terms of the Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International (CC BY-NC-ND 4.0) ( http://creativecommons.org/licenses/by-nc-nd/4.0/ ), which permits others to distribute the work, provided that the article is not altered or used commercially. You are not required to obtain permission to distribute this article, provided that you credit the author and journal.
- Cite this Page Lucier J, Dulebohn SC. Type 1 Diabetes. [Updated 2023 Mar 3]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-.
In this Page
Bulk download.
- Bulk download StatPearls data from FTP
Related information
- PMC PubMed Central citations
- PubMed Links to PubMed
Similar articles in PubMed
- Review Diabetes technology and treatments in the paediatric age group. [Int J Clin Pract Suppl. 2011] Review Diabetes technology and treatments in the paediatric age group. Shalitin S, Peter Chase H. Int J Clin Pract Suppl. 2011 Feb; (170):76-82.
- Continuous Subcutaneous Insulin Infusion (CSII) Pumps for Type 1 and Type 2 Adult Diabetic Populations: An Evidence-Based Analysis. [Ont Health Technol Assess Ser....] Continuous Subcutaneous Insulin Infusion (CSII) Pumps for Type 1 and Type 2 Adult Diabetic Populations: An Evidence-Based Analysis. Medical Advisory Secretariat. Ont Health Technol Assess Ser. 2009; 9(20):1-58. Epub 2009 Oct 1.
- The effectiveness of continuous subcutaneous insulin pumps with continuous glucose monitoring in outpatient adolescents with type 1 diabetes: A systematic review. [JBI Libr Syst Rev. 2012] The effectiveness of continuous subcutaneous insulin pumps with continuous glucose monitoring in outpatient adolescents with type 1 diabetes: A systematic review. Matsuda E, Brennan P. JBI Libr Syst Rev. 2012; 10(42 Suppl):1-10.
- Glycemic Control in Relation to Technology Use in a Single-Center Cohort of Children with Type 1 Diabetes. [Diabetes Technol Ther. 2022] Glycemic Control in Relation to Technology Use in a Single-Center Cohort of Children with Type 1 Diabetes. Sawyer A, Sobczak M, Forlenza GP, Alonso GT. Diabetes Technol Ther. 2022 Jun; 24(6):409-415. Epub 2022 Feb 16.
- Review Continuous glucose monitoring systems for type 1 diabetes mellitus. [Cochrane Database Syst Rev. 2012] Review Continuous glucose monitoring systems for type 1 diabetes mellitus. Langendam M, Luijf YM, Hooft L, Devries JH, Mudde AH, Scholten RJ. Cochrane Database Syst Rev. 2012 Jan 18; 1(1):CD008101. Epub 2012 Jan 18.
Recent Activity
- Type 1 Diabetes - StatPearls Type 1 Diabetes - StatPearls
Your browsing activity is empty.
Activity recording is turned off.
Turn recording back on
Connect with NLM
National Library of Medicine 8600 Rockville Pike Bethesda, MD 20894
Web Policies FOIA HHS Vulnerability Disclosure
Help Accessibility Careers
Advertisement
Genetics of type-1 diabetes
- Mini-Review
- Published: 02 September 2024
Cite this article

- Hiroshi Ikegami ORCID: orcid.org/0000-0001-8808-4605 1 , 2 &
- Shinsuke Noso 3
10 Accesses
Explore all metrics
Type-1 diabetes is a multifactorial disease characterized by genetic and environmental factors that contribute to its development and progression. Despite progress in the management of type-1 diabetes, the final goal of curing the disease is yet to be achieved. To establish effective methods for the prevention, intervention, and cure of the disease, the molecular mechanisms and pathways involved in its development and progression should be clarified. One effective approach is to identify genes responsible for disease susceptibility and apply information obtained from the function of genes in disease etiology for the protection, intervention, and cure of type-1 diabetes. In this review, we discuss the genetic basis of type-1 diabetes, along with prospects for its prevention, intervention, and cure for type-1 diabetes.
This is a preview of subscription content, log in via an institution to check access.
Access this article
Subscribe and save.
- Get 10 units per month
- Download Article/Chapter or eBook
- 1 Unit = 1 Article or 1 Chapter
- Cancel anytime
Price includes VAT (Russian Federation)
Instant access to the full article PDF.
Rent this article via DeepDyve
Institutional subscriptions

Similar content being viewed by others
Genetic approaches to the study of gene variants and their impact on the pathophysiology of type 2 diabetes.
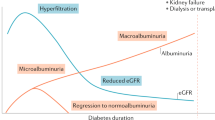
Genetics of diabetes mellitus and diabetes complications

Physiology Insights
Committee of the Japan Diabetes Society on the Diagnostic Criteria of Diabetes Mellitus; Seino Y, Nanjo K, Tajima N,et al. Report of the committee on the classification and diagnostic criteria of diabetes mellitus. Diabetol Int. 2010;1:2–20.
Kawasaki E, Maruyama T, Imagawa A, et al. Diagnostic criteria for acute-onset type 1 diabetes mellitus (2012): Report of the Committee of Japan Diabetes Society on the Research of Fulminant and Acute-onset Type 1 Diabetes Mellitus. Diabetol Int. 2013;4:221–5.
Article Google Scholar
Imagawa A, Hanafusa T, Awata T, et al. Report on the committee of the Japan Diabetes Society on the Research of fulminant and acute-onset type 1 diabetes mellitus: new diagnostic criteria of fulminant type 1 diabetes mellitus (2012). Diabetol Int. 2012;3:179–83.
Shimada A, Kawasaki E, Abiru N, et al. New diagnostic criteria (2023) for slowly progressive type 1 diabetes (SPIDDM): Report from Committee on Type 1 Diabetes of the Japan Diabetes Society (English version). Diabetol Int. 2024;15:1–4.
Article PubMed Google Scholar
Patterson C, Guariguata L, Dahlquist G, et al. Diabetes in the young - a global view and worldwide estimates of numbers of children with type 1 diabetes. Diabetes Res Clin Pract. 2014;103:161–75.
Imagawa A, Hanafusa T. Fulminant type 1 diabetes: a novel clinical entity requiring special attention by all medical practitioners. Nat Clin Prac Endocrinol Metab. 2007;3:36–45.
Ikegami H, Ogihara T. Genetics of insulin-dependent diabetes mellitus. Endocrine J. 1996;43:605–11.
Article CAS Google Scholar
Ikegami H, Kawabata Y, Noso S, et al. Genetics of type 1 diabetes in Asian and Caucasian populations. Diab Res Clin Prac. 2007;77(Suppl 1):S116–21.
Matsuda A, Kuzuya T. Diabetic twins in Japan. Diabetes Res Clin Pract. 1994;24(Suppl):S63–7.
Hyttinen V, Kaprio J, Kinnunen L, et al. Genetic liability of type 1 diabetes and the onset age among 22,650 young Finnish twin pairs: a nationwide follow-up study. Diabetes. 2003;52:1052–5.
Article CAS PubMed Google Scholar
Ikegami H, Makino S. The NOD mouse and its related strains. In: Sima AAF, Shafrir E, editors. Animal Models of Diabetes A Primer. Amsterdam: Harwood Academic Publishers; 2000. p. 43–61.
Google Scholar
Komeda K, Noda M, Terao K, et al. Establishment of two substrains, diabetes-prone and non-diabetic, from Long-Evans Tokushima Lean (LETL) rats. Endocr J. 1998;45:737–44.
Ikegami H, Makino S, Harada M, et al. The cataract Shionogi mouse, a sister strain of the non-obese diabetic mouse: similar class II but different class I gene products. Diabetologia. 1988;31:254–8.
Ikegami H, Yano N, Sato T, et al. Immunogenetics and immunopathogenesis of the NOD mouse. In: Eisenbarth GS, editor., et al., Immunotherapy of diabetes and selected autoimmune diseases. Boca Raton: CRC Press; 1989. p. 22–33.
Hattori M, Buse JB, Jackson RA, et al. The NOD mouse: recessive diabetogenic gene in the major histocompatibility complex. Science. 1986;231:733–5.
Wicker LS, Miller BJ, Coker LZ, et al. Genetic control of diabetes and insulitis in the nonobese diabetic (NOD) mouse. J Exp Med. 1987;165:1639–54.
Ikegami H, Makino S. Genetic susceptibility to insulin-dependent diabetes mellitus: from the NOD mouse to man. In: Shafrir E, editor. Frontiers in Diabetes Research: Lessons from Animal Diabetes IV. London: Smith-Gordon; 1993. p. 39–50.
Ikegami H, Makino S, Ogihara T. Molecular genetics of insulin-dependent diabetes mellitus: analysis of congenic strains. In: Shafrir E, editor. Frontiers in Diabetes Research: Lessons from Animal Diabetes VI. Boston: Birkhauser; 1996. p. 33–46.
Chapter Google Scholar
Kawabata Y, Ikegami H, Awata T, et al. Differential association of HLA with three subtypes of type 1 diabetes: fulminant, slowly progressive and acute-onset. Diabetologia. 2009;52:2513–21.
Awata T, Kawasaki E, Ikegami H, et al. Insulin gene/IDDM2 locus in Japanese type 1 diabetes: contribution of class I alleles and influence of class I subdivision in susceptibility to type 1 diabetes. J Clin Endocrinol Metab. 2007;92:1791–5.
Acha-Orbea H, McDevitt HO. The first external domain of the nonobese diabetic mouse class II I-A beta chain is unique. Proc Natl Acad Sci USA. 1987;84:2435–9.
Article CAS PubMed PubMed Central Google Scholar
Ikegami H, Eisenbarth GS, Hattori M. Major histocompatibility complex-linked diabetogenic gene of the nonobese diabetic mouse: analysis of genomic DNA amplified by the polymerase chain reaction. J Clin Invest. 1990;85:18–24.
Ikegami H, Makino S, Yamato E, et al. Identification of a new susceptibility locus for insulin-dependent diabetes mellitus by ancestral haplotype congenic mapping. J Clin Invest. 1995;96:1936–42.
Inoue K, Ikegami H, Fujisawa T, et al. Allelic variation in class I K gene as candidate for second component of MHC-linked susceptibility to type 1 diabetes in NOD mouse. Diabetologia. 2004;47:739–47.
Hattori M, Yamato E, Itoh N, et al. Cutting edge: homologous recombination of the MHC class I K region defines new MHC-linked diabetogenic susceptibility gene(s) in nonobese diabetic mice. J Immunol. 1999;163:1721–4.
Awata T, Kuzuya T, Matsuda A, et al. Genetic analysis of HLA class II alleles and susceptibility to type 1 (insulin-dependent) diabetes mellitus in Japanese subjects. Diabetologia. 1992;35:419–24.
Ikegami H, Kawaguchi Y, Yamato E, et al. Analysis by the polymerase chain reaction of histocompatibility leucocyte antigen-DR9-linked susceptibility to insulin-dependent diabetes mellitus. J Clin Endocrinol Metab. 1992;75:1381–5.
CAS PubMed Google Scholar
Kawabata Y, Ikegami H, Kawaguchi Y, et al. Asian-specific HLA haplotypes reveal heterogeneity of the contribution of HLA-DR and -DQ haplotypes to susceptibility to type 1 diabetes. Diabetes. 2002;51:545–51.
Fujisawa T, Ikegami H, Yamato E, et al. Class I HLA is associated with age-at-onset of IDDM, while class II HLA confers susceptibility to IDDM. Diabetologia. 1995;38:1494.
Kawabata Y, Ikegami H, Kawaguchi Y, et al. Age-related association of MHC class I chain-related gene A (MICA) with type I (insulin-dependent) diabetes mellitus. Hum Immunol. 2000;61:624.
Nejentsev S, Howson JM, Walker NM, et al. Localization of type 1 diabetes susceptibility to the MHC class I genes HLA-B and HLA-A. Nature. 2007;450:887–92.
Julier C, Hyer RN, Davies J, et al. Insulin-IGF2 region on chromosome 11p encodes a gene implicated in HLA-DR4-dependent diabetes susceptibility. Nature. 1991;354:155–9.
Lucassen AM, Julier C, Beressi JP, et al. Susceptibility to insulin dependent diabetes mellitus maps to a 4.1kb segment of DNA spanning the insulin gene and associated with VNTR. Nat Genet. 1993;4:305–10.
Kawaguchi Y, Ikegami H, Shen G-Q, et al. Insulin gene region contributes to genetic susceptibility to, but may not to low incidence of, insulin-dependent diabetes mellitus in Japanese. Biochem Biophys Res Commun. 1997;233:283–7.
Vafiadia P, Bennett ST, Todd JA, et al. Insulin expression in human thymus is modulated by INS VNTR alleles at the IDDM2 locus. Nat Genet. 1997;15:289–92.
Pugliese A, Zeller M, Fernandez A Jr, et al. The insulin gene is transcribed in the human thymus and transcription levels correlate with allelic variation at the INS VNTR-IDDM2 susceptibility locus for type 1 diabetes. Nat Genet. 1997;15:293–6.
Nakayama M, Abiru N, Moriyama H, et al. Prime role for an insulin epitope in the development of type 1 diabetes in NOD mice. Nature. 2005;435:220–3.
Noso S, Kataoka K, Kawabata Y, et al. Insulin transactivator MafA regulates intra-thymic expression of insulin and affects susceptibility to type 1 diabetes. Diabetes. 2010;59:2579–87.
Noso S, Kawabata Y, Babaya N, et al. Association study of MAFA and MAFB, genes related to organ-specific autoimmunity, with susceptibility to type 1 diabetes in Japanese and Caucasian populations. J Genet Syndr Gene Ther. 2013;4:204.
Bottini N, Musumeci L, Alonso A, et al. A functional variant of lymphoid tyrosine phosphatase is associated with type 1 diabetes. Nat Genet. 2004;36:337–8.
Ueda H, Howson JMM, Esposito L, et al. Association of the T-cell regulatory gene CTLA4 with susceptibility to autoimmune disease. Nature. 2003;423:506–11.
Lowe CE, Cooper JD, Brusko T, et al. Large-scale genetic fine mapping and genotype-phenotype associations implicate polymorphism in the IL2RA region in type 1 diabetes. Nat Genet. 2007;39:1074–82.
Ikegami H, Awata T, Kawasaki E, et al. The association of CTLA4 polymorphism with type 1 diabetes is concentrated in patients complicated with autoimmune thyroid disease: a multi-center collaborative study in Japan. J Clin Endocrinol Metab. 2006;91:1087–92.
Kawasaki E, Awata T, Ikegami H, et al. Systematic search for single nucleotide polymorphisms in a lymphoid tyrosine phosphatase (PTPN22) gene: Association between promoter polymorphism and type 1 diabetes in Asian populations. Am J Med Genet. 2006;140:586–93.
Awata T, Kawasaki E, Tanaka S, et al. Association of type 1 diabetes with two loci on 12q13 and 16p13 and the influence coexisting thyroid autoimmunity in Japanese. J Clin Endocrinol Metab. 2009;94:231–5.
Kawasaki E, Awata T, Ikegami H, et al. Genetic association between the IL2RA and mode of onset of type 1 diabetes in the Japanese population. J Clin Endocrinol Metab. 2009;94:947–52.
Yamashita H, Awata T, Kawasaki E, et al. Analysis of the HLA and non-HLA susceptibility loci in Japanese type 1 diabetes. Diabetes Metab Res Rev. 2011;27:844–8.
Ikegami H, Noso S, Babaya N, et al. Genetic basis of type 1 diabetes: similarities and differences between East and West. Rev Diabet Stud. 2008;5:64–72.
Article PubMed PubMed Central Google Scholar
Sirugo G, Williams SM, Tishkoff SA. The missing diversity in human genetic studies. Cell. 2019;177(1):26–31.
All of Us Research Program Genomics Investigators. Genomic data in the All of Us Research Program. Nature. 2024;627:340-6. https://doi.org/10.1038/s41586-023-06957-x . Online ahead of print.
Davies JL, Kawaguchi Y, Bennett ST, et al. A genome-wide search for human type 1 diabetes susceptibility genes. Nature. 1994;371:130–6.
Todd JA, Walker NM, Cooper JD, et al. Robust associations of four new chromosome regions from genome-wide analyses of type 1 diabetes. Nat Genet. 2007;39:857–64.
Barrett JC, Clayton DG, Concannon P, et al. Genome-wide association study and meta-analysis find that over 40 loci affect risk of type 1 diabetes. Nat Genet. 2009;41:703–7.
Chiou J, Geusz RJ, Okino ML, et al. Interpreting type 1 diabetes risk with genetics and single-cell epigenomics. Nature. 2021;594:398–402.
Robertson CC, Inshaw JRJ, Onengut-Gumuscu S, et al. Fine-mapping, trans-ancestral and genomic analyses identify causal variants, cells, genes and drug targets for type 1 diabetes. Nat Genet. 2021;53:962–71.
Todd JA, Mijovic C, Fletcher J, et al. Identification of susceptibility loci for insulin-dependent diabetes mellitus by trans-racial gene mapping. Nature. 1989;338:587–9.
Ikegami H, Noso S, Babaya N, et al. Genetics and pathogenesis of type 1 diabetes: prospects for prevention and intervention. J Diabetes Investig. 2011;2:415–20.
Kawabata Y, Nishida N, Awata T, et al. A genome-wide association study confirming a strong effect of HLA and identifying variants in CSAD/lnc-ITGB7–1 on chromosome 12q13.13 associated with susceptibility to fulminant type 1 diabetes. Diabetes. 2019;68:665–75.
Kawabata Y, Ikegami H. Genetics of fulminant type 1 diabetes. Diabetol Int. 2020;11:315–22.
Arany E, Strutt B, Romanus P, et al. Taurine supplement in early life altered islet morphology, decreased insulitis and delayed the onset of diabetes in non-obese diabetic mice. Diabetologia. 2004;47:1831–7.
Lin S, Yang J, Wu G, et al. Inhibitory effects of taurine on STZ-induced apoptosis of pancreatic islet cells. Adv Exp Med Biol. 2013;775:287–97.
Nakatsuru Y, Murase-Mishiba B-T M, et al. Taurine improves glucose tolerance in STZ-induced insulin-deficient diabetic mice. Diabetol Int. 2018;9:234–42.
Noso S, Babaya N, Hiromine Y, et al. Metabolic signatures of β-cell destruction in type 1 diabetes. J Diabetes Investig. 2023;14:48–57.
Sun BB, Kurki MI, Foley CN, et al. Genetic associations of protein-coding variants in human disease. Nature. 2022;603:95–102.
Olson ND, Wagner J, Dwarshuis N, et al. Variant calling and benchmarking in an era of complete human genome sequences. Nat Rev Genet. 2023;24:464–83.
Kishi A, Kawabata Y, Ugi S, et al. The onset of diabetes in three out of four sisters: a Japanese family with type 1 diabetes. a case report. Endocr J. 2009;56:767–72.
Ina Y, Kawabata Y, Sakamoto R, et al. A rare HLA genotype in two siblings with type 1 diabetes in a Japanese family clustered with type 1 diabetes. J Diabetes Investig. 2017;8:762–5.
Ikegami H. Molecular genetics of type 1 diabetes. J Jpn Diabetes Soc. 2024;67:1–7.
Noso S, Hosomichi K, Babaya N, et al. Whole-exome sequencing in rare families identified novel genetic variants for familial type 1 diabetes. Diabetologia. 2017;60(Suppl1):S24–5.
Ikegami H, Babaya N, Noso S. Beta-cell failure in diabetes: common susceptibility and mechanisms shared between type 1 and type 2 diabetes. J Diabetes Investig. 2021;12:1526–39.
Willyard C. Can autoimmune diseases be cured? Scientists see hope at last Nature. 2024;625:646–8.
CAS Google Scholar
Dolgin E. How a pioneering diabetes drug offers hope for preventing autoimmune disorders. Nature. 2023;614:404–6.
Uno S, Imagawa A, Kozawa J, et al. Complete loss of insulin secretion capacity in type 1A diabetes patients during long-term follow up. J Diabetes Investig. 2018;9:806–12.
Keenan HA, Sun JK, Levine J, et al. Residual insulin production and pancreatic ß-cell turnover after 50 years of diabetes: Joslin Medalist Study. Diabetes. 2010;59:2846–53.
Niwano F, Babaya N, Hiromine Y, et al. Glucose metabolism after pancreatectomy: opposite extremes between pancreaticoduodenectomy and distal pancreatectomy. J Clin Endocrinol Metab. 2021;106:e2203–14.
Niwano F, Babaya N, Hiromine Y, et al. Three-year observation of glucose metabolism after pancreaticoduodenectomy: A single-center prospective study in Japan. J Clin Endocrinol Metab. 2022;107:3362–9.
Imamura S, Niwano F, Babaya N, et al. High incidence of diabetes mellitus after distal pancreatectomy and its predictors: A long-term follow-up study. J Clin Endocrinol Metab. 2024;109:619-30. https://doi.org/10.1210/clinem/dgad634 .
Baumel-Alterzon S, Katz LS, Brill G, et al. Nrf2: the master and captain of beta cell fate. Trends Endocrinol Metab. 2021;32:7–19.
Meyerovich K, Ortis F, Allagnat F, et al. Endoplasmic reticulum stress and the unfolded protein response in pancreatic islet inflammation. J Mol Endocrinol. 2016;57:R1–17.
Hotta M, Tashiro F, Ikegami H, Niwa H, Ogihara T, Yodoi J, Miyazaki J-I. Pancreatic beta-cell-specific expression of thioredoxin, an antioxidative and anti-apoptotic protein, prevents autoimmune and streptozotocin-induced diabetes. J Exp Med. 1998;188:1445–51.
Yamamoto M, Yamato E, Shu-Ichi T, Tashiro F, Ikegami H, Yodoi J, Miyazaki J. Transgenic Expression of Antioxidant Protein Thioredoxin in Pancreatic β Cells Prevents Progression of Type 2 Diabetes Mellitus. Antioxid Redox Sig. 2008;10:43–50.
Ikegami H, Fujisawa T, Ogihara T. Mouse models of type 1 and type 2 diabetes derived from the same closed colony: genetic susceptibility shared between two types of diabetes? ILAR J. 2004;45:267–76.
Dooley J, Tian L, Schonefeldt S, et al. Genetic predisposition for beta cell fragility underlies type 1 and type 2 diabetes. Nat Genet. 2016;48:519–27.
Rutsch N, Chamberlain CE, Dixon W, et al. Diabetes with multiple autoimmune and inflammatory conditions linked to an activating SKAP2 mutation. Diabetes Care. 2021;44:1816–25.
Hebbar P, Nizam R, John SE, et al. Linkage analysis using whole exome sequencing data implicates SLC17A1, SLC17A3, TATDN2 and TMEM131L in type 1 diabetes in Kuwaiti families. Sci Rep. 2023;13:14978.
Download references
Author information
Authors and affiliations.
Professor Emeritus, Kindai University, Osaka-sayama, Japan
Hiroshi Ikegami
Director of Health Administration Center and Nikkei Clinic, Human Resources, Nikkei Inc. Osaka Head Office, Osaka, Japan
Department of Endocrinology, Metabolism and Diabetes, Faculty of Medicine, Kindai University, Osaka-sayama, Japan
Shinsuke Noso
You can also search for this author in PubMed Google Scholar
Corresponding author
Correspondence to Hiroshi Ikegami .
Ethics declarations
Conflict of interest.
Hiroshi Ikegami: lecture fees (Novo Nordisk Pharma, Sanofi, Sumitomo Pharma), scholarship donations (LifeScan Japan, Sumitomo Pharma).
Additional information
Publisher's note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
About this article
Ikegami, H., Noso, S. Genetics of type-1 diabetes. Diabetol Int (2024). https://doi.org/10.1007/s13340-024-00754-1
Download citation
Received : 13 March 2024
Accepted : 06 August 2024
Published : 02 September 2024
DOI : https://doi.org/10.1007/s13340-024-00754-1
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Find a journal
- Publish with us
- Track your research
New Study Examines the Impact of Periods on Type 1 Diabetes

Diabetes Center Berne and Tidepool are recruiting for a study that examines the menstrual cycle in people with type 1 diabetes. Participants will receive financial compensation.
Trial Name: DCB x Tidepool Menstrual Cycle Study
Diabetes Type: Type 1 diabetes
Trial Sponsor: Diabetes Center Berne
What is the study researching?
Diabetes Center Berne (DCB), a Swiss foundation that aims to identify unmet needs in diabetes technology, is working on a study with the nonprofit diabetes app developer Tidepool which is collecting data from the Tidepool data platform from women in the U.S. with type 1 diabetes.
The study objectives are to identify changes in blood glucose levels and insulin requirements throughout the menstrual cycle for people with type 1 diabetes, better understand the relationship between menstrual periods and insulin-dependent diabetes, and support the development of solutions to reduce the amount of user input required, ultimately lowering the burden of diabetes management throughout the menstrual cycle.
Why is this study important?
DCB researchers noticed that women with diabetes often said their hormonal cycles had an impact on blood glucose management, but there have been few published studies to date with sufficient data.
Martina Rothenbühler, DCB’s scientific program manager, said that she plans to analyze data on the entire female menstrual cycle. The goal is for any new insights from the study to help develop tailored treatment strategies for menstruating people facing diabetes challenges every month.
“It’s vital to offer young women diagnosed with diabetes some perspective, support and tools that will help them navigate the disease throughout their lives,” Rothenbühler added.
What does the study entail?
Participation in this project will involve completing a questionnaire about your diabetes management and reproductive history.
If you are eligible for this study, you will be asked to upload anywhere from four to 12 months of CGM, insulin pump, and menstrual cycle data. You will need to provide consent for the project collaborators to use your anonymized data for research. Note that you will need to be at a computer to fill out the screener and upload your data.
The study’s data is fully anonymized, which means neither DCB nor Tidepool will have access to any personal identifying information connected to your diabetes data. Once you have completed the study, you will receive a $100 Mastercard gift card.
Find more information about the project here .
Are you interested in participating?

You may be eligible if you:
- Are a resident of the U.S.
- Are living with type 1 diabetes and are 18 or older
- Currently have a menstrual cycle
- Use a CGM as well as an insulin pump or a smart pen for most of your insulin delivery
- Are willing to share anonymized diabetes data and menstrual cycle data
To enroll or learn more about this study, visit the Menstrual Cycle Study homepage and/or email [email protected] . If you have questions about how diabetes data will be anonymized during the study, email Tidepool’s support team at [email protected] .
More coverage of the intersection between women’s health and diabetes:
- Harnessing the Power of Periods for A1C Testing
- How Does Menopause Affect Diabetes?
- Does PCOS Raise the Risk for Type 2 Diabetes?
Photo credits: iStock (top); courtesy Tidepool (bottom).
Weekly insulin injection as effective as daily injections in type 1 and type 2 diabetes, research suggests

Shutterstock.com
A once-weekly injection of insulin is as effective as daily injections for blood sugar management in both type 1 and type 2 diabetes mellitus (T1DM/T2DM), studies have suggested.
In a phase 3, non-inferior study, published in The Lancet on 10 September 2024 , 692 adults with T1DM were randomly assigned to receive either once-weekly insulin efsitora (n=343) or once-daily insulin degludec (n=349), both in combination with insulin lispro.
The study aimed to assess the efficacy and safety of efsitora compared with degludec by measuring the change in glycated haemoglobin (HbA1c) and incidence of severe hypoglycaemia during the 52-week study period.
At week 26, researchers found that mean HbA1c decreased from 7.88% (62.66 mmol/mol) at baseline to 7.41% (57.5 mmol/mol) with efsitora, compared with 7.94% (63.3 mmol/mol) at baseline to 7.36% (56.9 mmol/mol) with degludec — a mean change of -0.51% with efsitora and -0.56% with degludec — confirming a non-inferiority margin of 0.4% for efsitora compared with degludec.
However, the incidence rate of moderate or severe hypoglycaemia with efsitora compared with degludec was 14.03 versus 11.59 events per patient-year of exposure — an increased risk of 21%, which was statistically significant.
The incidence of severe hypoglycaemia was also reported more frequently in the efsitora cohort at 10% (n=35/343), compared with degludec at 3% (n=11/349), during the 52-week period. Hypoglycaemia was reported more frequently in the first 12 weeks of the trial.
The authors noted that while efsitora showed non-inferior HbA 1c reduction compared with degludec, the greater incidence of severe hypoglycaemia in participants treated with efsitora may “suggest the need for additional evaluation of efsitora dose initiation and optimisation in people with type 1 diabetes”.
Another phase 3, non-inferior study, published on 10 September 2024 in the New England Journal of Medicine , included 928 participants with T2DM, who were randomly assigned to receive either efsitora (n=466) or degludec (n=462) over 52 weeks.
At week 52, researchers found that mean HbA1c decreased from 8.21% at baseline to 6.97% with efsitora (−1.26 percentage points) and from 8.24% to 7.05% with degludec (−1.17 percentage points), with an estimated treatment difference of −0.09 percentage points, demonstrating non-inferiority of the weekly injection.
The T2DM study also observed an incidence rate of moderate or severe hypoglycaemia with efsitora compared with degludec at 0.58 versus 0.45 events per participant-year of exposure; however, these findings were not statistically significant.
Commenting on the studies, Philip Newland-Jones, consultant pharmacist in diabetes and endocrinology at University Hospital Southampton NHS Foundation Trust, said: “Once-weekly insulin has the potential to support in those patients who have insulin resistance in T2DM and require similar background doses of insulin daily.
“There are possible groups that may benefit from once-weekly dosing, such as those requiring district nurses; however, there are also potential risks to take into consideration in this group,” he added.
“I believe that in line with data for insulin icodec once-weekly insulin, these data confirm that these insulins are unlikely to be used widely in T2DM because of the increased risk of hypoglcyaemic episodes compared with standard care.
“This is likely to be due to the differing daily requirements and flexibility in insulin required in the management of T1DM, further highlighting the benefits of hybrid closed-loop insulin systems, which can vary background insulin requirements,” explained Newland-Jones.
Similar to insulin efsitora, insulin icodec is a once-weekly injection, which is currently under review for regulatory approval for treatment of T2DM . However, it has also been associated with an increased risk of hypoglycaemia.
Guidance from the National Institute for Health and Care Excellence on icodec is expected to be published in May 2025.
Also commenting on the studies, Katie Bareford, senior clinical advisor at Diabetes UK, said: “Keeping blood sugars in target range with insulin therapy can be relentless and exhausting.
“A reduction in the number of insulin injections could lessen the burden of living with diabetes and better support people in their efforts to manage their diabetes.
“We welcome these findings and look forward to further research on once-weekly insulin injections to ensure they are safe and effective for everyone who could benefit,” she said.
Please leave a comment Cancel reply
You must be logged in to post a comment.
You may also be interested in

Test your knowledge of diabetes

Almost one-third of people on low-calorie diet programme in remission from type 2 diabetes mellitus, study results show

Number of patients at risk of type 2 diabetes increases by half a million in one year
Changing our Future Through Research
The ADA is committed to innovation and breakthrough research that will improve the lives of all people living with diabetes.

ADA Research: Science. Progress. Hope.
ADA research provides critical funding for diabetes research. With 100% of donations directed to research, our goal is to ensure adequate financial resources to support innovative scientific discovery that will translate to life-changing treatments and eventual cures.
of our funded researchers remain dedicated to careers in diabetes science
publications per grant, cited an average of 28 times, proving expertise and credibility
Every $1 the ADA invests in diabetes research leads to $12.47 in additional research funding
ADA Research Impact
Explore some of the latest innovations and discoveries and see how the ADA continues to advance science, leverage investments and retain scientists.

Research Funds at Work
Imagine what 290 scientists, each working on a unique project at 117 institutions across the U.S. can do. Learn about the research we fund to move the diabetes fight forward.

Helping People Thrive
Uncover inspiring patient stories and find out how our research is transforming lives.

Discover programs on research, career development, training, and more.
Learn more about the current opportunities for 2024 research funding.
Pathway to Stop Diabetes ®
A bold initiative dedicated to bringing 100 brilliant scientists to diabetes research.
Explore Research Projects
As part of our mission, ADA’s Research Programs invest in projects that have the potential to prevent the development of diabetes and help people living with diabetes.

Type 1 Diabetes Research
Project topics span technology, islet transplantation, immunology, improving transition to self-management, and more.

Type 2 Diabetes Research
Project topics include support for potential new treatments, a better understating of genetic factors, addressing disparities, and more.

Prediabetes/Insulin Resistance Research
Projects include understanding the role of exercise, novel therapies, and more.

Gestational Diabetes Research
Projects focus on advancing the prevention of gestational diabetes and to properly diagnose and treat it when it occurs.

Research on Obesity
Projects include studying the biology of appetite regulation and metabolism, identification of new treatment targets, and trials exploring interventions for weight loss.

Give Today and Change lives!
With your support, the American Diabetes Association® can continue our lifesaving work to make breakthroughs in research and provide people with the resources they need to fight diabetes.
- Alzheimer's disease & dementia
- Arthritis & Rheumatism
- Attention deficit disorders
- Autism spectrum disorders
- Biomedical technology
- Diseases, Conditions, Syndromes
- Endocrinology & Metabolism
- Gastroenterology
- Gerontology & Geriatrics
- Health informatics
- Inflammatory disorders
- Medical economics
- Medical research
- Medications
- Neuroscience
- Obstetrics & gynaecology
- Oncology & Cancer
- Ophthalmology
- Overweight & Obesity
- Parkinson's & Movement disorders
- Psychology & Psychiatry
- Radiology & Imaging
- Sleep disorders
- Sports medicine & Kinesiology
- Vaccination
- Breast cancer
- Cardiovascular disease
- Chronic obstructive pulmonary disease
- Colon cancer
- Coronary artery disease
- Heart attack
- Heart disease
- High blood pressure
- Kidney disease
- Lung cancer
- Multiple sclerosis
- Myocardial infarction
- Ovarian cancer
- Post traumatic stress disorder
- Rheumatoid arthritis
- Schizophrenia
- Skin cancer
- Type 2 diabetes
- Full List »
share this!
September 12, 2024
This article has been reviewed according to Science X's editorial process and policies . Editors have highlighted the following attributes while ensuring the content's credibility:
fact-checked
trusted source
Fear of hypoglycemia remains a major barrier to exercise among adults with type 1 diabetes, research shows
by Diabetologia

Despite high use of continuous glucose monitoring and insulin pump therapy, fear of hypoglycemia (low blood sugar) remains a significant barrier to physical activity and exercise for adults with type 1 diabetes (T1D), according to new research presented at the Annual Meeting of The European Association for the Study of Diabetes ( EASD ), held in Madrid (9–13 Sept).
However, the findings suggest that if exercise and diabetes management are discussed in the clinic, this fear could be reduced.
"Regular exercise can help individuals with diabetes to achieve their blood glucose goals, improve their body composition and fitness, as well as reduce their risk of heart attacks and strokes, which is higher in people with type 1 diabetes," explained lead author Dr. Catriona Farrell from the University of Dundee, Scotland, UK.
"Yet many people living with type 1 diabetes do not maintain a healthy body weight or manage to do the recommended amount of physical activity each week."
A number of previous studies have examined barriers to exercise in T1D, but these have been limited by their small sample size.
To fill this important evidence gap, researchers from the University of Dundee assessed knowledge and barriers to physical activity in adults with T1D and associated predictive factors.
Adults with T1D were recruited from the NHS Research Scotland Diabetes Network (research register) and internationally via social media.
Overall, 463 adults, 221 men and 242 women, with T1D answered an anonymous web-based questionnaire to assess barriers to physical activity (measured on the modified Barriers to Physical Activity in type 1 Diabetes [BAPAD-1] scale), diabetes management, and attitudes to exercise and sport.
Participants were asked to rate on a 7-point Likert scale (1, extremely unlikely to 7, extremely likely) the chance that each of 13 factors would keep them from doing regular physical activity in the next six months. Factors included: loss of control over diabetes, the risk of hypoglycemia, the fear of being tired, the fear of getting hurt, a low fitness level, and lack of social support.
Researchers calculated average scores for each factor and assessed which were most correlated with perceived barriers to physical activity, as well as identifying independent predictors.
The participant reported median age of respondents was 45–54 years, median disease duration 21–25 years, and median HbA1c 50–55 mmol/mol (an ideal level is 48 mmol/mol or below).
Over three-quarters (79%) of respondents reported using continuous or flash glucose monitoring, around two-thirds (64%) said they were treated with multiple daily insulin injections, and over a third (36%) reported using insulin pump therapy.
The researchers identified that despite advances in technologies and diabetes management , risk of hypoglycemia with exercise remains a significant barrier to physical activity.
Importantly, participants who best understood the importance of adjusting insulin dose before and after exercise as well as adjusting carbohydrate intake for exercise were found to be less fearful of hypoglycemia associated with physical activity. This knowledge is essential in order to adapt insulin and/or carbohydrate intake to prevent hypoglycemia induced by exercise.
The researchers also found that being asked about exercise or sport within a diabetes clinic was negatively correlated with fear of hypoglycemia, and identified exercise confidence as the strongest independent predictor of fear of physical activity.
"Our findings demonstrate that in order to break down the barriers to physical activity, and empower our patients to exercise safely and effectively, we need to improve the education we provide and our dialogue about exercise in clinics," said Dr. Farrell.
"In turn, this should help them to achieve the multitude of health benefits that exercise offers."
Explore further
Feedback to editors

Reprogramming cancer cells to attack themselves
6 minutes ago

AI-based tissue staining can detect amyloid deposits without chemical stains or polarization microscopy
14 minutes ago

Mucin gel may help disk herniation patients after surgery
26 minutes ago

Nested premotor circuits activity found to drive male flies' production of distinct courtship songs
27 minutes ago

Scientists discover key features of language sites that could help preserve function after brain surgery
4 hours ago

Long-term metastatic melanoma survival dramatically improves on immunotherapy, clinical trial finds
Sep 15, 2024

Team discovers role of ferroptosis in combating breast cancer resistance
Sep 13, 2024

Metformin found to reduce organ aging in male monkeys

Researchers discover new target for treating heart failure: Protein kinase N

RNA-sequencing study provides novel insights into chronic lymphocytic leukemia
Related stories.

Study reveals best types of exercise for patients with diabetes
Aug 21, 2024

ACSM updates guidance for exercise in type 2 diabetes
Feb 16, 2022

Many people with type 1 diabetes continue to struggle to control blood sugar surrounding exercise
Jun 15, 2023

Artificial pancreas can prevent dangerously low blood sugar in people with T1D
Aug 27, 2020

How people with type 2 diabetes can get the benefits of exercise while reducing the risks
Nov 19, 2019

Mini-dose glucagon may halt post-exercise hypoglycemia
May 30, 2018
Recommended for you

Machine learning could help reduce hospitalizations by nearly 30% during a pandemic, study finds

Increased testing for heart disease indicator needed worldwide, say experts

Avian flu found in wastewater of 10 Texas cities through virome sequencing
Sep 12, 2024

Automated insulin delivery technology helps marathon runners with type 1 diabetes

Conversations between clinicians and their patients about firearms could save lives

Study finds doctors and patients interested in environmental impact of health care decisions
Let us know if there is a problem with our content.
Use this form if you have come across a typo, inaccuracy or would like to send an edit request for the content on this page. For general inquiries, please use our contact form . For general feedback, use the public comments section below (please adhere to guidelines ).
Please select the most appropriate category to facilitate processing of your request
Thank you for taking time to provide your feedback to the editors.
Your feedback is important to us. However, we do not guarantee individual replies due to the high volume of messages.
E-mail the story
Your email address is used only to let the recipient know who sent the email. Neither your address nor the recipient's address will be used for any other purpose. The information you enter will appear in your e-mail message and is not retained by Medical Xpress in any form.
Newsletter sign up
Get weekly and/or daily updates delivered to your inbox. You can unsubscribe at any time and we'll never share your details to third parties.
More information Privacy policy
Donate and enjoy an ad-free experience
We keep our content available to everyone. Consider supporting Science X's mission by getting a premium account.
E-mail newsletter
Study reveals how SARS-CoV-2 triggers diabetes by destroying pancreatic cells
- Download PDF Copy
Researchers from Weill Cornell Medicine have used a cutting-edge model system to uncover the mechanism by which SARS-CoV-2, the virus that causes COVID-19, induces new cases of diabetes, and worsens complications in people who already have it. The team found that viral exposure activates immune cells that in turn destroy beta (β) cells, the pancreatic cells that produce insulin. The study was published Sept. 2 in Cell Stem Cell.
There has long been a hypothesis in the field that certain viral infections may trigger type 1 diabetes. But we were able to show how this happens in the context of COVID-19 infection." Dr. Shuibing Chen, co-corresponding author, director of the Center for Genomic Health, the Kilts Family Professor of Surgery and a member of the Hartman Institute for Therapeutic Organ Regeneration at Weill Cornell Medicine
"When someone has severe COVID-19, of course the first priority is to treat the life-threatening symptoms," said co-corresponding author Dr. Robert Schwartz, an associate professor of medicine at Weill Cornell Medicine and a gastroenterologist and hepatologist at NewYork-Presbyterian/Weill Cornell Medical Center. "But moving forward, there may be a way to develop clinical therapeutics that help avoid later injury to organs like the pancreas."
Dr. Liuliu Yang and Dr. Yuling Han, who were postdoctoral fellows in the Department of Surgery, and Dr. Tuo Zhang, an instructor in microbiology and immunology at Weill Cornell Medicine, were co-first authors of the paper.
From the early days of the COVID-19 pandemic, doctors caring for sick patients observed that the virus affected a number of organ systems, including not only the lungs, but also the heart, liver, colon and pancreas. For the current work, the researchers started with samples of pancreatic tissue from autopsies of people who had died of COVID-19. They observed that the pancreatic islets, the parts of the pancreas that generate the insulin to regulate blood sugar, were damaged.
Related Stories
- Flight altitude changes may affect blood glucose levels of type 1 diabetes patients using insulin pumps
- Night owls have higher BMI, larger waists and face higher risk of type 2 diabetes
- Obesity increases risk of contracting COVID-19 after exposure to SARS-CoV-2
They then used an analysis technique called GeoMx to study the samples in more detail. This revealed the presence of immune cells called proinflammatory macrophages in the tissues. The job of these macrophages is to kill off pathogens, but they sometimes cause collateral damage to healthy tissues.
To learn more about this activity, the team used a model system developed in the Chen Lab that had never been used before; pancreatic islet organoids (mini organs) that included both a vascular system and immune cells. "If we want to use organoids to study how a disease progresses, it's important to be able to include components of the immune system in these models," said Dr. Chen. In this case, after infecting the organoids with SARS-CoV-2, they found the macrophages appeared to be killing off the β cells through a type of cell death called pyroptosis.
The team also used the organoids to study how the pancreas responds to infection with another infectious virus — coxsackievirus B4, which has been implicated in the onset of type 1 diabetes. They found a similar macrophage response. "Moving forward, this organoid system is going to be useful for looking at other viruses as well," Dr. Schwartz said.
Further research on the signaling molecules that activate the macrophages also suggested potential interventions for protecting β cells from damage in patients with severe infections. Although it is too early to begin testing any treatments, this is something that may be possible in the future. This work could also help shed light on the underlying causes of long COVID, a condition that is believed to affect more than 15 million people in the United States.
Weill Cornell Medicine
Yang, L., et al . (2024). Human vascularized macrophage-islet organoids to model immune-mediated pancreatic β cell pyroptosis upon viral infection. Cell Stem Cell . doi.org/10.1016/j.stem.2024.08.007 .
Posted in: Medical Science News | Medical Research News | Medical Condition News | Disease/Infection News
Tags: Blood , Blood Sugar , Cell , Cell Death , Colon , covid-19 , Diabetes , Genomic , Heart , Immune System , Immunology , Insulin , Kidney , Liver , Lungs , Macrophage , Medicine , Microbiology , Organoids , Pancreas , Pandemic , Research , SARS , SARS-CoV-2 , Surgery , Therapeutics , Type 1 Diabetes , Vascular , Virus
Suggested Reading

Cancel reply to comment
- Trending Stories
- Latest Interviews
- Top Health Articles

How can microdialysis benefit drug development
Ilona Vuist
In this interview, discover how Charles River uses the power of microdialysis for drug development as well as CNS therapeutics.

Global and Local Efforts to Take Action Against Hepatitis
Lindsey Hiebert and James Amugsi
In this interview, we explore global and local efforts to combat viral hepatitis with Lindsey Hiebert, Deputy Director of the Coalition for Global Hepatitis Elimination (CGHE), and James Amugsi, a Mandela Washington Fellow and Physician Assistant at Sandema Hospital in Ghana. Together, they provide valuable insights into the challenges, successes, and the importance of partnerships in the fight against hepatitis.

Addressing Important Cardiac Biology Questions with Shotgun Top-Down Proteomics
In this interview conducted at Pittcon 2024, we spoke to Professor John Yates about capturing cardiomyocyte cell-to-cell heterogeneity via shotgun top-down proteomics.

Latest News

Newsletters you may be interested in
Your AI Powered Scientific Assistant
Hi, I'm Azthena, you can trust me to find commercial scientific answers from News-Medical.net.
A few things you need to know before we start. Please read and accept to continue.
- Use of “Azthena” is subject to the terms and conditions of use as set out by OpenAI .
- Content provided on any AZoNetwork sites are subject to the site Terms & Conditions and Privacy Policy .
- Large Language Models can make mistakes. Consider checking important information.
Great. Ask your question.
Azthena may occasionally provide inaccurate responses. Read the full terms .
While we only use edited and approved content for Azthena answers, it may on occasions provide incorrect responses. Please confirm any data provided with the related suppliers or authors. We do not provide medical advice, if you search for medical information you must always consult a medical professional before acting on any information provided.
Your questions, but not your email details will be shared with OpenAI and retained for 30 days in accordance with their privacy principles.
Please do not ask questions that use sensitive or confidential information.
Read the full Terms & Conditions .
Provide Feedback


IMAGES
VIDEO
COMMENTS
Type 1 diabetes (also known as diabetes mellitus) is an autoimmune disease in which immune cells attack and destroy the insulin-producing cells of the pancreas. The loss of insulin leads to the ...
Type 1 diabetes is an autoimmune condition resulting in insulin deficiency and eventual loss of pancreatic β cell function requiring lifelong insulin therapy. Since the discovery of insulin more than 100 years ago, vast advances in treatments have improved care for many people with type 1 diabetes. Ongoing research on the genetics and immunology of type 1 diabetes and on interventions to ...
Although research into type 1 diabetes prevention and disease modification continues to produce encouraging data, none of the approaches discussed above appears sufficiently effective alone in preventing or managing type 1 diabetes. Future endeavours will, therefore, require a novel focus, leveraging prior experience with regard to the ...
Type 1 Research Highlights. While the Association's priority is to improve the lives of all people affected by diabetes, type 1 diabetes is a critical focus of the organization. In fact, in 2016, 37 percent of our research budget was dedicated to projects relevant to type 1 diabetes. Read more about the critical research made possible by the ...
The burden of type 1 diabetes remains substantial, and more research is needed to improve the lives of people with type 1 diabetes and to find a cure. To this end, ADA-funded research continues to drive progress by funding research projects topics spanning technology, islet transplantation, immunology, improving transition to self-management ...
2. Type 1 Diabetes Mellitus. Type 1 diabetes mellitus (T1DM) incidence has been increasing by 2-5% worldwide with significant heterogeneity in this diagnosis by regions or continents [5,6].Clinical care has significantly improved, raising quality of life and clinical outcomes for these patients, but more must be done to find a cure.
The burden of type 1 diabetes in 2021 is vast and is expected to increase rapidly, especially in resource-limited countries. Most incident and prevalent cases are adults. The substantial missing prevalence highlights the premature mortality of type 1 diabetes and an opportunity to save and extend lives of people with type 1 diabetes. Our new model, which will be made publicly available as the ...
Type 1 diabetes is a chronic autoimmune disease that requires lifelong care including requiring insulin, either through multiple daily injections or continuous infusion using a pump, every day to ...
Hummel, S. et al. Children diagnosed with presymptomatic type 1 diabetes through public health screening have milder diabetes at clinical manifestation. Diabetologia 66 , 1633-1642 (2023).
Hypoglycaemia is a common occurrence in people with type 1 diabetes mellitus, and can have serious consequences. This Review defines hypoglycaemia in type 1 diabetes mellitus, and also outlines ...
Abstract. Type 1 diabetes is a chronic autoimmune disease characterised by insulin deficiency and resultant hyperglycaemia. Knowledge of type 1 diabetes has rapidly increased over the past 25 years, resulting in a broad understanding about many aspects of the disease, including its genetics, epidemiology, immune and β-cell phenotypes, and ...
Over several decades, studies have described the progression of autoimmune diabetes, from the first appearance of autoantibodies until, and after, the diagnosis of clinical disease with hyperglycaemia and insulin dependence. Despite the improved management of type 1 diabetes with exogenous insulin, most patients do not meet clinical glycaemic goals, and diabetes remains an important medical ...
Join the movement to end T1D. Champion federal funding for T1D research. Inform health and regulatory policy. Improve lives. Breakthrough T1D is the leading global type 1 diabetes (T1D) research and advocacy organization. As we drive toward curing type 1 diabetes, we help make everyday life better for the people who face it.
Type 1 diabetes is an autoimmune disease that causes the body's immune system to attack and destroy insulin-producing beta cells in the pancreas. Traditional management of type 1 diabetes has primarily involved replacing the missing insulin with injections which, though effective, can be expensive and burdensome. ... The research centers on a ...
Promising early results show that longstanding Harvard Stem Cell Institute (HSCI) research may have paved the way for a breakthrough treatment of Type 1 diabetes. Utilizing research from the Melton Lab, Vertex Pharmaceuticals has developed VX-880, an investigational stem cell-derived, fully differentiated pancreatic islet cell replacement therapy for people with type 1 diabetes (T1D).
A focus of type 1 diabetes research is preventing the autoimmune destruction of the pancreatic β cell. 166 Primary strategies to prevent the onset of autoimmunity in infants at high risk for developing type 1 diabetes by modifying diet or introducing supplements in early life have not succeeded. 167-169 Antigen-specific immunotherapy has ...
There are about 1.5 million adults with Type 1 diabetes in the U.S., compared to 21 million adults with Type 2 diabetes. In terms of the total cases of diabetes, only 5 to 10 percent have Type 1 diabetes. Even in our largest epidemiologic cohorts, only a small percentage of people have Type 1 diabetes. So, we just don't have the same national ...
Type 1 diabetes is caused by an autoimmune attack of insulin-producing beta-cells. While genetics and the environment are known to play important roles, the underlying factors explaining why the immune system mistakenly recognize beta-cells as foreign is not known. Now, Dr. Delong has discovered a potential explanation.
Type 1 diabetes, once known as juvenile diabetes or insulin-dependent diabetes, is a chronic condition. In this condition, the pancreas makes little or no insulin. ... Even after a lot of research, type 1 diabetes has no cure. Treatment is directed toward managing the amount of sugar in the blood using insulin, diet and lifestyle to prevent ...
Type 1 diabetes mellitus (T1D) is an autoimmune disease that leads to the destruction of insulin-producing pancreatic beta cells. There is heterogeneity in the metabolic, genetic, and immunogenetic characteristics of T1D and age-related differences, requiring a personalized approach for each individual. Loss of insulin secretion can occur quickly or gradually. Residual insulin production ...
DRI clinical trials are already dramatically improving the lives of some people with type 1 diabetes who are now living insulin-free. The Institute's scientists are addressing the major research challenges that stand in the way of a biological cure. But continuing this research is only possible with your support.
Type-1 diabetes is a multifactorial disease characterized by genetic and environmental factors that contribute to its development and progression. Despite progress in the management of type-1 diabetes, the final goal of curing the disease is yet to be achieved. To establish effective methods for the prevention, intervention, and cure of the disease, the molecular mechanisms and pathways ...
Type 1 diabetes is a chronic (life-long) autoimmune disease that prevents your pancreas from making insulin. It requires daily management with insulin injections. ... Type 1 Diabetes TrialNet, an international research network, also offers autoantibody testing to family members of people with Type 1 diabetes. The presence of autoantibodies ...
Diabetes Center Berne and Tidepool are recruiting for a study that examines the menstrual cycle in people with type 1 diabetes. Participants will receive financial compensation. Diabetes Center Berne (DCB), a Swiss foundation that aims to identify unmet needs in diabetes technology, is working on a ...
A once-weekly injection of insulin is as effective as daily injections for blood sugar management in both type 1 and type 2 diabetes mellitus (T1DM/T2DM), studies have suggested. In a phase 3, non-inferior study, published in The Lancet on 10 September 2024, 692 adults with T1DM were randomly assigned to receive either once-weekly insulin efsitora […]
Type 1 Diabetes Research Project topics span technology, islet transplantation, immunology, improving transition to self-management, and more. See Project Examples Type 2 Diabetes Research Project topics include support for potential new treatments, a better understating of genetic factors, addressing disparities, and more. ...
Citation: Fear of hypoglycemia remains a major barrier to exercise among adults with type 1 diabetes, research shows (2024, September 12) retrieved 13 September 2024 from https://medicalxpress.com ...
There has long been a hypothesis in the field that certain viral infections may trigger type 1 diabetes. But we were able to show how this happens in the context of COVID-19 infection ...
Type 1 diabetes can occur at any age, and a significant proportion is diagnosed during adulthood. Latent autoimmune diabetes of adults (LADA) is the diagnostic term applied when type 1 diabetes develops in adults; it has a slower onset than the same condition in children. Given this difference, some use the unofficial term "type 1.5 diabetes ...